Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0315 - Recurrent Bleeding Gastrointestinal Angioectasias and Acquired Von Willebrand Deficiency (Heyde’s Syndrome) Developing in the Setting of Mild Hypertrophic Obstructive Cardiomyopathy
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- RM
Ravi Moghe, DO
Ohiohealth Doctors Hospital
Columbus, OH
Presenting Author(s)
Ravi Moghe, DO1, Andrew Volio, DO2, Kristin Lescalleet, DO1, Musa Abu-Jubara, DO1, Levi Atinda, DO1, Zeryab Khan, DO1, Robert Palma, DO1
1Ohiohealth Doctors Hospital, Columbus, OH; 2Ohiohealth Doctors Hopsital, Columbus, OH
Introduction: Heyde’s Syndrome is classically described as a triad of gastrointestinal arteriovenous malformations, aortic stenosis (AS), and acquired von Willebrand syndrome (aVWS). Acknowledged as under-diagnosed, the syndrome is frequently missed even in the presence of classically associated moderate-to-severe AS. Perhaps compounding diagnostic difficulty are more recent reports of alternative forms of structural heart disease, including hypertrophic obstructive cardiomyopathy (HOCM), that, although rarer, are capable of producing the syndrome as well.
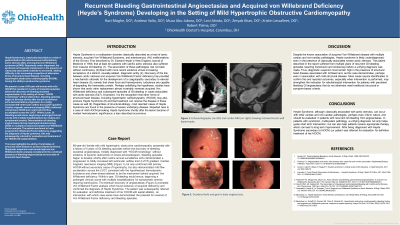
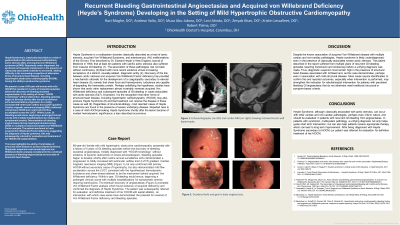
Case Description/Methods: 68-year-old woman with mild hypertrophic obstructive cardiomyopathy that resulted in 5 years of gastrointestinal bleeding episodes before the discovery of bleeding duodenal angioectasias. Initially diagnosed with “HOCM morphology” without evidence of dynamic obstruction on stress echocardiogram, bleeding episodes began to develop shortly after routine annual surveillance echo demonstrated a progression to mildly increased left ventricular outflow tract (LVOT) gradient. Cardiac magnetic resonance imaging (MRI) not only confirmed mild primary HOCM without secondary cause of hypertrophy, but also demonstrated mild flow acceleration across the LVOT, consistent with the hypothesized hemodynamic turbulence and sheer-stress believed to be the mechanism behind acquired von Willebrand deficiency. Within a year, gastrointestinal bleeding would ensue, beginning a prolonged clinical course with multiple hospitalizations for symptomatic anemia requiring transfusions. The eventual discovery of angioectasias prompted von Willebrand Factor analysis which found evidence of acquired deficiency and confirmed the diagnosis of Heyde Syndrome. The patient was subsequently referred for evaluation and definitive treatment of her HOCM with septal ablation, an intervention with which case series have demonstrated the potential for reversal of von Willebrand Factor deficiency and bleeding episodes.
Discussion: Often a delayed diagnosis owing to the seemingly disparate constellation of findings in Heyde’s, this particular case additionally highlights that even more mild states of structural heart disease can provoke the syndrome outside of previously reported severe structural disease. Diagnostic suspicion must remain high and von Willebrand factor analysis considered in the combined presence of GI bleed and mild cardiomyopathy and valvulopathy.
Disclosures:
Ravi Moghe, DO1, Andrew Volio, DO2, Kristin Lescalleet, DO1, Musa Abu-Jubara, DO1, Levi Atinda, DO1, Zeryab Khan, DO1, Robert Palma, DO1. D0315 - Recurrent Bleeding Gastrointestinal Angioectasias and Acquired Von Willebrand Deficiency (Heyde’s Syndrome) Developing in the Setting of Mild Hypertrophic Obstructive Cardiomyopathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Ohiohealth Doctors Hospital, Columbus, OH; 2Ohiohealth Doctors Hopsital, Columbus, OH
Introduction: Heyde’s Syndrome is classically described as a triad of gastrointestinal arteriovenous malformations, aortic stenosis (AS), and acquired von Willebrand syndrome (aVWS). Acknowledged as under-diagnosed, the syndrome is frequently missed even in the presence of classically associated moderate-to-severe AS. Perhaps compounding diagnostic difficulty are more recent reports of alternative forms of structural heart disease, including hypertrophic obstructive cardiomyopathy (HOCM), that, although rarer, are capable of producing the syndrome as well.
Case Description/Methods: 68-year-old woman with mild hypertrophic obstructive cardiomyopathy that resulted in 5 years of gastrointestinal bleeding episodes before the discovery of bleeding duodenal angioectasias. Initially diagnosed with “HOCM morphology” without evidence of dynamic obstruction on stress echocardiogram, bleeding episodes began to develop shortly after routine annual surveillance echo demonstrated a progression to mildly increased left ventricular outflow tract (LVOT) gradient. Cardiac magnetic resonance imaging (MRI) not only confirmed mild primary HOCM without secondary cause of hypertrophy, but also demonstrated mild flow acceleration across the LVOT, consistent with the hypothesized hemodynamic turbulence and sheer-stress believed to be the mechanism behind acquired von Willebrand deficiency. Within a year, gastrointestinal bleeding would ensue, beginning a prolonged clinical course with multiple hospitalizations for symptomatic anemia requiring transfusions. The eventual discovery of angioectasias prompted von Willebrand Factor analysis which found evidence of acquired deficiency and confirmed the diagnosis of Heyde Syndrome. The patient was subsequently referred for evaluation and definitive treatment of her HOCM with septal ablation, an intervention with which case series have demonstrated the potential for reversal of von Willebrand Factor deficiency and bleeding episodes.
Discussion: Often a delayed diagnosis owing to the seemingly disparate constellation of findings in Heyde’s, this particular case additionally highlights that even more mild states of structural heart disease can provoke the syndrome outside of previously reported severe structural disease. Diagnostic suspicion must remain high and von Willebrand factor analysis considered in the combined presence of GI bleed and mild cardiomyopathy and valvulopathy.
Disclosures:
Ravi Moghe indicated no relevant financial relationships.
Andrew Volio indicated no relevant financial relationships.
Kristin Lescalleet indicated no relevant financial relationships.
Musa Abu-Jubara indicated no relevant financial relationships.
Levi Atinda indicated no relevant financial relationships.
Zeryab Khan indicated no relevant financial relationships.
Robert Palma indicated no relevant financial relationships.
Ravi Moghe, DO1, Andrew Volio, DO2, Kristin Lescalleet, DO1, Musa Abu-Jubara, DO1, Levi Atinda, DO1, Zeryab Khan, DO1, Robert Palma, DO1. D0315 - Recurrent Bleeding Gastrointestinal Angioectasias and Acquired Von Willebrand Deficiency (Heyde’s Syndrome) Developing in the Setting of Mild Hypertrophic Obstructive Cardiomyopathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
