Back

Poster Session C - Monday Afternoon
Category: IBD
C0436 - Extraintestinal Manifestations of Ulcerative Colitis Presenting as Tracheobronchitis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Brittney Shupp, DO
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Brittney Shupp, DO, Zarian Prenatt, DO, Brian Kim, DO, Neal Fitzpatrick, MD, Berhanu Geme, MD
St. Luke's University Health Network, Bethlehem, PA
Introduction: Ulcerative Colitis (UC) is an inflammatory condition primarily involving the colon but is commonly associated with different extraintestinal manifestations. However, pulmonary manifestations, specifically tracheal involvement, in UC is extremely rare with only a few documented cases in the literature to date. We present a case of pulmonary manifestations of UC presenting as a chronic cough in a patient with UC status post colectomy.
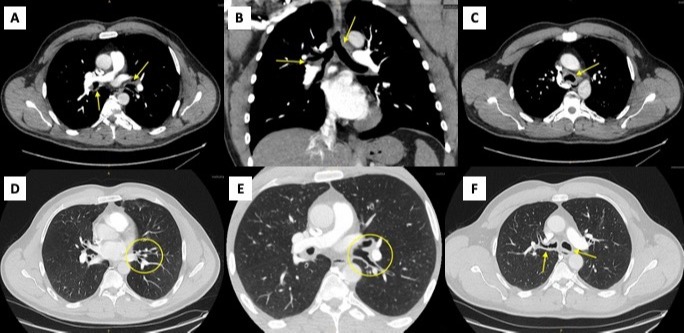
Case Description/Methods: A 54-year-old male with a past medical history of GERD, reflux laryngitis, and UC status post total colectomy with J-pouch 10 years prior presented to his primary care provider’s office with the complaint of persistent shortness of breath. Associated symptoms included hoarseness and a chronic cough with thick sputum production and chest tightness. On examination, the patient had extensive wheezing and thus was instructed to utilize an albuterol inhaler and was prescribed a 10-day prednisone taper. Following completion of the prescribed regimen, the patient’s chest tightness and dyspnea improved but his hoarseness and cough persisted. The patient was therefore started on Fluticasone Furoate-Vilanteril 100-25 mcg/inhalation and sent for chest imaging. CT chest was completed and revealed moderate, concentric thickening of the trachea and walls of the bronchi and bronchioles. There was no evidence of parenchymal disease or serositis, but findings were very suspicious for pulmonary UC involvement (Image 1). Following initiation of Fluticasone Furoate-Vilanteril, the patient did have moderate improvement in symptoms. However, considering the CT imaging findings, the decision was made to increase the dosage to Fluticasone Furoate-Vilanteril 200-25 mcg/inhalation to allow for inflammatory suppression over the course of next couple of months.
Discussion: Bronchopulmonary involvement only occurs in 0.21 to 0.4% of all inflammatory bowel disease (IBD) cases, and there are less than 20 documented cases of tracheobronchitis in patients with UC in the literature to date. Few of these cases have occurred in patients whose IBD have been in remission or have undergone total colectomies the year prior. Fortunately, pulmonary involvement in UC responds favorably to corticosteroids often resulting in quick improvement both clinically and radiographically. However, given its manifesting symptoms, patients can be easily misdiagnosed with asthma or COPD if physicians do not have a high index of suspicion.
Disclosures:
Brittney Shupp, DO, Zarian Prenatt, DO, Brian Kim, DO, Neal Fitzpatrick, MD, Berhanu Geme, MD. C0436 - Extraintestinal Manifestations of Ulcerative Colitis Presenting as Tracheobronchitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
St. Luke's University Health Network, Bethlehem, PA
Introduction: Ulcerative Colitis (UC) is an inflammatory condition primarily involving the colon but is commonly associated with different extraintestinal manifestations. However, pulmonary manifestations, specifically tracheal involvement, in UC is extremely rare with only a few documented cases in the literature to date. We present a case of pulmonary manifestations of UC presenting as a chronic cough in a patient with UC status post colectomy.
Case Description/Methods: A 54-year-old male with a past medical history of GERD, reflux laryngitis, and UC status post total colectomy with J-pouch 10 years prior presented to his primary care provider’s office with the complaint of persistent shortness of breath. Associated symptoms included hoarseness and a chronic cough with thick sputum production and chest tightness. On examination, the patient had extensive wheezing and thus was instructed to utilize an albuterol inhaler and was prescribed a 10-day prednisone taper. Following completion of the prescribed regimen, the patient’s chest tightness and dyspnea improved but his hoarseness and cough persisted. The patient was therefore started on Fluticasone Furoate-Vilanteril 100-25 mcg/inhalation and sent for chest imaging. CT chest was completed and revealed moderate, concentric thickening of the trachea and walls of the bronchi and bronchioles. There was no evidence of parenchymal disease or serositis, but findings were very suspicious for pulmonary UC involvement (Image 1). Following initiation of Fluticasone Furoate-Vilanteril, the patient did have moderate improvement in symptoms. However, considering the CT imaging findings, the decision was made to increase the dosage to Fluticasone Furoate-Vilanteril 200-25 mcg/inhalation to allow for inflammatory suppression over the course of next couple of months.
Discussion: Bronchopulmonary involvement only occurs in 0.21 to 0.4% of all inflammatory bowel disease (IBD) cases, and there are less than 20 documented cases of tracheobronchitis in patients with UC in the literature to date. Few of these cases have occurred in patients whose IBD have been in remission or have undergone total colectomies the year prior. Fortunately, pulmonary involvement in UC responds favorably to corticosteroids often resulting in quick improvement both clinically and radiographically. However, given its manifesting symptoms, patients can be easily misdiagnosed with asthma or COPD if physicians do not have a high index of suspicion.
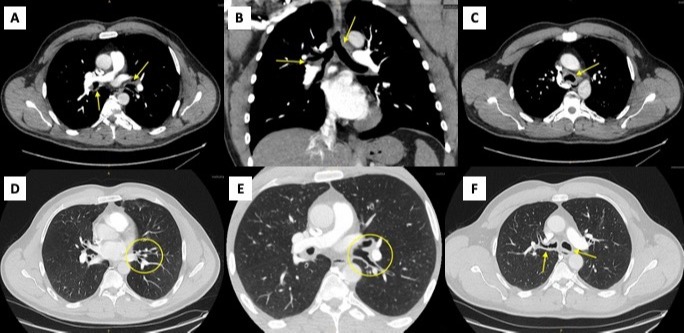
Figure: Image 1 A-F: Moderate concentric thickening of the wall of the trachea and diffuse thickening of the walls of the bronchi and bronchioles. Overall findings highly suspicious for airway involvement of ulcerative colitis.
Disclosures:
Brittney Shupp indicated no relevant financial relationships.
Zarian Prenatt indicated no relevant financial relationships.
Brian Kim indicated no relevant financial relationships.
Neal Fitzpatrick indicated no relevant financial relationships.
Berhanu Geme indicated no relevant financial relationships.
Brittney Shupp, DO, Zarian Prenatt, DO, Brian Kim, DO, Neal Fitzpatrick, MD, Berhanu Geme, MD. C0436 - Extraintestinal Manifestations of Ulcerative Colitis Presenting as Tracheobronchitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
