Back


Poster Session C - Monday Afternoon
Category: Esophagus
C0257 - “Outpouchings in the Esophagus:” A Rare Case of HIV-Associated Esophageal Intramural Pseudodiverticulosis in the Absence of Esophageal Candidiasis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Daniyal Raza, MD
Louisiana State University Health Sciences Center
Shreveport, LA
Presenting Author(s)
Daniyal Raza, MD, Maryam Mubashir, MD, Meher Sindhoora Mavuram, MD, Hassaan A. Zia, MD
Louisiana State University Health Sciences Center, Shreveport, LA
Introduction:
Esophageal Intramural Pseudodiverticulosis (EIP) is a benign condition that presents with dysphagia. EIP with HIV AIDS is rare, especially in the absence of concomitant esophageal candidiasis. We present a case of dysphagia in a patient with HIV, found to have EIP.
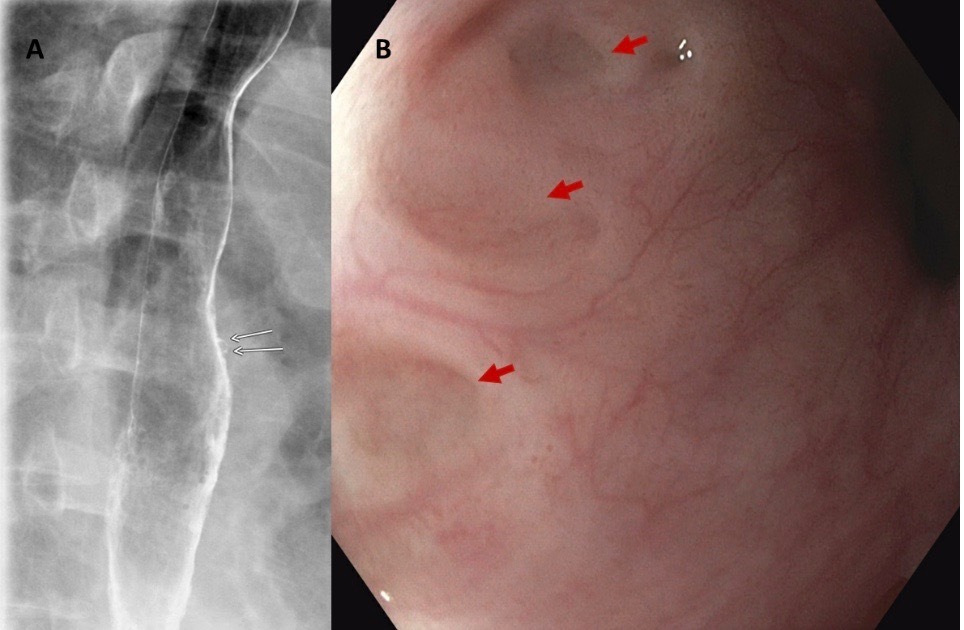
Case Description/Methods: 51-year-old African American female with AIDS and noncompliance to Highly Active Antiretroviral Therapy (HAART) and a CD4 count of 0.5 cells/ mm3, presented with a 3-month history of progressively worsening dysphagia, to solids and liquids, odynophagia, and retrosternal burning. A barium esophagogram demonstrated an intramural pseudodiverticula. On upper endoscopy, multiple diminutive pseudo diverticula were visualized with no other gross abnormalities, including ulcers or stenoses (Figure B). Pathology from esophageal biopsies showed chronic inflammatory changes with no fungal or viral elements identified. The patient was re-initiated on HAART and high dose proton pump inhibitors with complete resolution of dysphagia on follow up.
Discussion: The pathogenesis of EIP involves esophageal excretory ductal obstruction and submucosal fibrosis from chronic inflammation and duct dilation from dysmotility. Risk factors include HIV, diabetes mellitus, esophageal candidiasis, chronic alcohol abuse, Mallory-Weiss syndrome, Crohn’s disease, GERD, corrosive esophageal injury and esophageal malignancies. Single contrast barium esophagogram remains the study of choice and demonstrated numerous 1–4 mm flask-shaped diverticula. An upper endoscopy can be performed to corroborate imaging findings and diagnose concomitant structural and infectious etiologies. Management includes PPI therapy, treatment of underlying etiology, and dilation of any stenoses. Surveillance endoscopy can be considered due to an association with esophageal malignancies. The association of HIV with EIP, especially in the absence of esophageal candidiasis, is rarely reported. Clinicians should consider EIP as part of the differential diagnosis for HIV patients presenting with dysphagia.
Disclosures:
Daniyal Raza, MD, Maryam Mubashir, MD, Meher Sindhoora Mavuram, MD, Hassaan A. Zia, MD. C0257 - “Outpouchings in the Esophagus:” A Rare Case of HIV-Associated Esophageal Intramural Pseudodiverticulosis in the Absence of Esophageal Candidiasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Louisiana State University Health Sciences Center, Shreveport, LA
Introduction:
Esophageal Intramural Pseudodiverticulosis (EIP) is a benign condition that presents with dysphagia. EIP with HIV AIDS is rare, especially in the absence of concomitant esophageal candidiasis. We present a case of dysphagia in a patient with HIV, found to have EIP.
Case Description/Methods: 51-year-old African American female with AIDS and noncompliance to Highly Active Antiretroviral Therapy (HAART) and a CD4 count of 0.5 cells/ mm3, presented with a 3-month history of progressively worsening dysphagia, to solids and liquids, odynophagia, and retrosternal burning. A barium esophagogram demonstrated an intramural pseudodiverticula. On upper endoscopy, multiple diminutive pseudo diverticula were visualized with no other gross abnormalities, including ulcers or stenoses (Figure B). Pathology from esophageal biopsies showed chronic inflammatory changes with no fungal or viral elements identified. The patient was re-initiated on HAART and high dose proton pump inhibitors with complete resolution of dysphagia on follow up.
Discussion: The pathogenesis of EIP involves esophageal excretory ductal obstruction and submucosal fibrosis from chronic inflammation and duct dilation from dysmotility. Risk factors include HIV, diabetes mellitus, esophageal candidiasis, chronic alcohol abuse, Mallory-Weiss syndrome, Crohn’s disease, GERD, corrosive esophageal injury and esophageal malignancies. Single contrast barium esophagogram remains the study of choice and demonstrated numerous 1–4 mm flask-shaped diverticula. An upper endoscopy can be performed to corroborate imaging findings and diagnose concomitant structural and infectious etiologies. Management includes PPI therapy, treatment of underlying etiology, and dilation of any stenoses. Surveillance endoscopy can be considered due to an association with esophageal malignancies. The association of HIV with EIP, especially in the absence of esophageal candidiasis, is rarely reported. Clinicians should consider EIP as part of the differential diagnosis for HIV patients presenting with dysphagia.
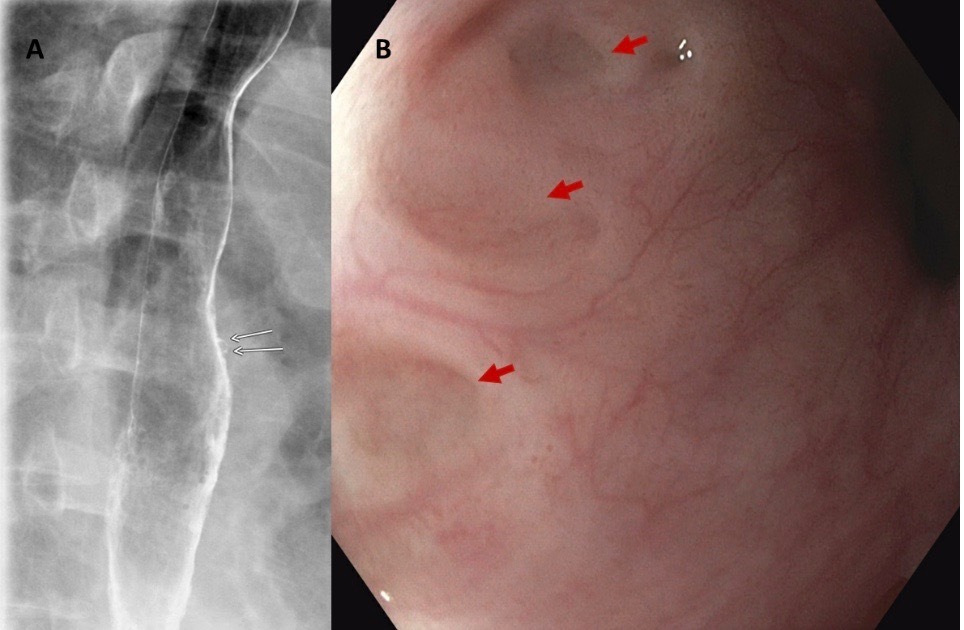
Figure: Figure A. Barium esophagogram shows psuedodiverticula (white arrows)
Figure B. Pseudodiverticula seen on upper endoscopy (red arrows)
Figure B. Pseudodiverticula seen on upper endoscopy (red arrows)
Disclosures:
Daniyal Raza indicated no relevant financial relationships.
Maryam Mubashir indicated no relevant financial relationships.
Meher Sindhoora Mavuram indicated no relevant financial relationships.
Hassaan Zia indicated no relevant financial relationships.
Daniyal Raza, MD, Maryam Mubashir, MD, Meher Sindhoora Mavuram, MD, Hassaan A. Zia, MD. C0257 - “Outpouchings in the Esophagus:” A Rare Case of HIV-Associated Esophageal Intramural Pseudodiverticulosis in the Absence of Esophageal Candidiasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
