Back

Poster Session B - Monday Morning
Category: Liver
B0596 - Flood Syndrome: A Challenge for the Clinician
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Paola Morocho, MD
University of Connecticut Health Center
Farmington, Connecticut
Presenting Author(s)
Aida Roman, MD, MS1, Erica C. Becker, MD, MPH1, Paola Morocho, MD1, Patrick Troy, MD, MS2
1University of Connecticut Health Center, Farmington, CT; 2Pulmonary and Critical Care Medicine Hartford HealthCare Medical Group, Hartford, CT
Introduction: Flood syndrome is a rare life-threatening complication of spontaneous paracentesis from a ruptured umbilical hernia typically in the setting of refractory ascites and end-stage liver cirrhosis. While conservative management is associated with higher mortality compared to surgical management, herniorrhaphy in patients with end-stage liver cirrhosis remains difficult to plan due to a high-risk of morbidity and mortality. We present a case of flood syndrome and our multidisciplinary approach for management.
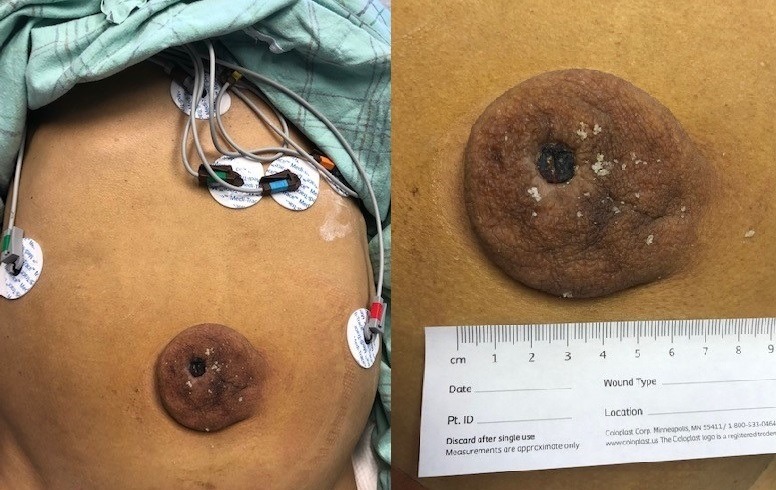
Case Description/Methods: A 59-year-old male, with decompensated alcoholic cirrhosis including esophageal varices, recurrent ascites, and hepatocellular carcinoma, presented with hepatic encephalopathy and a ruptured umbilical hernia leaking ascites. He was hemodynamically stable and afebrile. His MELD-Na score on admission was 30. A CT abdomen was negative for incarcerated hernia or obstruction. After obtaining cultures he was started on cefepime and vancomycin. Additionally, he received albumin 25g every 6 hours, lactulose and rifaximin. Medical and surgical planning included evaluation by gastroenterology, infectious disease, and surgery for medical optimization with the aim of pursuing elective repair when the patient was at his lowest MELD score. Unfortunately, he deteriorated clinically with worsening encephalopathy and hemodynamic instability. Ultimately, he was considered too unstable for herniorrhaphy. His hospital course was complicated by Staphylococcus lugdunensis and vancomycin-resistant Enterococcus faecium peritonitis and sepsis despite multiple antimicrobials. He eventually developed a massive rectal bleed and transitioned to comfort measures per family wishes.
Discussion: Flood syndrome has a poor prognosis with a high mortality rate. Patients with end-stage liver disease and recurrent ascites are at higher risk due to increased intra-abdominal pressure, weakened abdominal muscle and fascia, and malnutrition. There is no standard of care for management of flood syndrome, but literature favors early surgical intervention. Our case shows the difficulty and complexity of managing these patients. Despite utilization of a multidisciplinary approach to care for our patient, the severity of our patient’s liver disease and his frailty made him ineligible for surgical intervention. Early surgical intervention to prevent rupture of these umbilical hernias may ensure the best chance at positive patient outcomes.
Disclosures:
Aida Roman, MD, MS1, Erica C. Becker, MD, MPH1, Paola Morocho, MD1, Patrick Troy, MD, MS2. B0596 - Flood Syndrome: A Challenge for the Clinician, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2Pulmonary and Critical Care Medicine Hartford HealthCare Medical Group, Hartford, CT
Introduction: Flood syndrome is a rare life-threatening complication of spontaneous paracentesis from a ruptured umbilical hernia typically in the setting of refractory ascites and end-stage liver cirrhosis. While conservative management is associated with higher mortality compared to surgical management, herniorrhaphy in patients with end-stage liver cirrhosis remains difficult to plan due to a high-risk of morbidity and mortality. We present a case of flood syndrome and our multidisciplinary approach for management.
Case Description/Methods: A 59-year-old male, with decompensated alcoholic cirrhosis including esophageal varices, recurrent ascites, and hepatocellular carcinoma, presented with hepatic encephalopathy and a ruptured umbilical hernia leaking ascites. He was hemodynamically stable and afebrile. His MELD-Na score on admission was 30. A CT abdomen was negative for incarcerated hernia or obstruction. After obtaining cultures he was started on cefepime and vancomycin. Additionally, he received albumin 25g every 6 hours, lactulose and rifaximin. Medical and surgical planning included evaluation by gastroenterology, infectious disease, and surgery for medical optimization with the aim of pursuing elective repair when the patient was at his lowest MELD score. Unfortunately, he deteriorated clinically with worsening encephalopathy and hemodynamic instability. Ultimately, he was considered too unstable for herniorrhaphy. His hospital course was complicated by Staphylococcus lugdunensis and vancomycin-resistant Enterococcus faecium peritonitis and sepsis despite multiple antimicrobials. He eventually developed a massive rectal bleed and transitioned to comfort measures per family wishes.
Discussion: Flood syndrome has a poor prognosis with a high mortality rate. Patients with end-stage liver disease and recurrent ascites are at higher risk due to increased intra-abdominal pressure, weakened abdominal muscle and fascia, and malnutrition. There is no standard of care for management of flood syndrome, but literature favors early surgical intervention. Our case shows the difficulty and complexity of managing these patients. Despite utilization of a multidisciplinary approach to care for our patient, the severity of our patient’s liver disease and his frailty made him ineligible for surgical intervention. Early surgical intervention to prevent rupture of these umbilical hernias may ensure the best chance at positive patient outcomes.
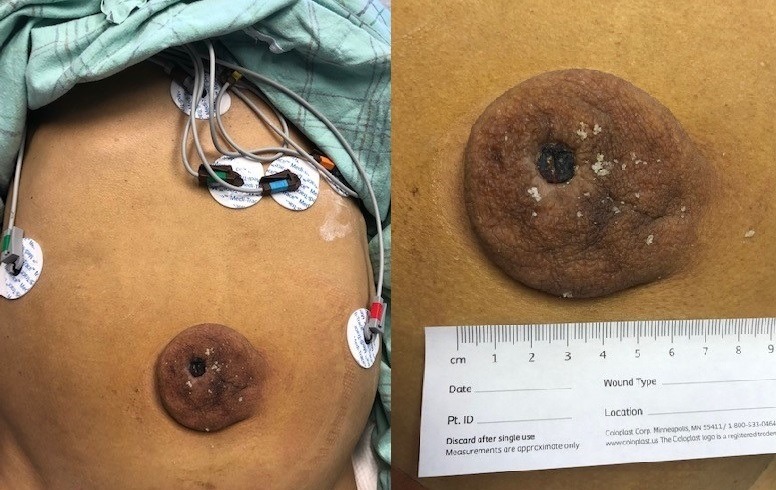
Figure: A. Large 6.5cm umbilical hernia
Disclosures:
Aida Roman indicated no relevant financial relationships.
Erica Becker indicated no relevant financial relationships.
Paola Morocho indicated no relevant financial relationships.
Patrick Troy indicated no relevant financial relationships.
Aida Roman, MD, MS1, Erica C. Becker, MD, MPH1, Paola Morocho, MD1, Patrick Troy, MD, MS2. B0596 - Flood Syndrome: A Challenge for the Clinician, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
