Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0237 - Incidental Acute Esophageal Necrosis in a Post-Cholecystectomy Patient
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- JC
Jacqueline P. Chang, MD
Oregon Health & Science University
Portland, OR
Presenting Author(s)
Jacqueline P. Chang, MD, Eric R. Yoo, MD, Jessica Yu, MD, MS
Oregon Health & Science University, Portland, OR
Introduction: Acute esophageal necrosis (AEN), or “black esophagus”, is a rare clinical entity characterized by diffuse, black mucosal discoloration of the esophagus on endoscopy. Patients often present with hematemesis, shock, and melena. The condition has a relatively high mortality rate due to the comorbid conditions that are frequently present at the time of diagnosis.
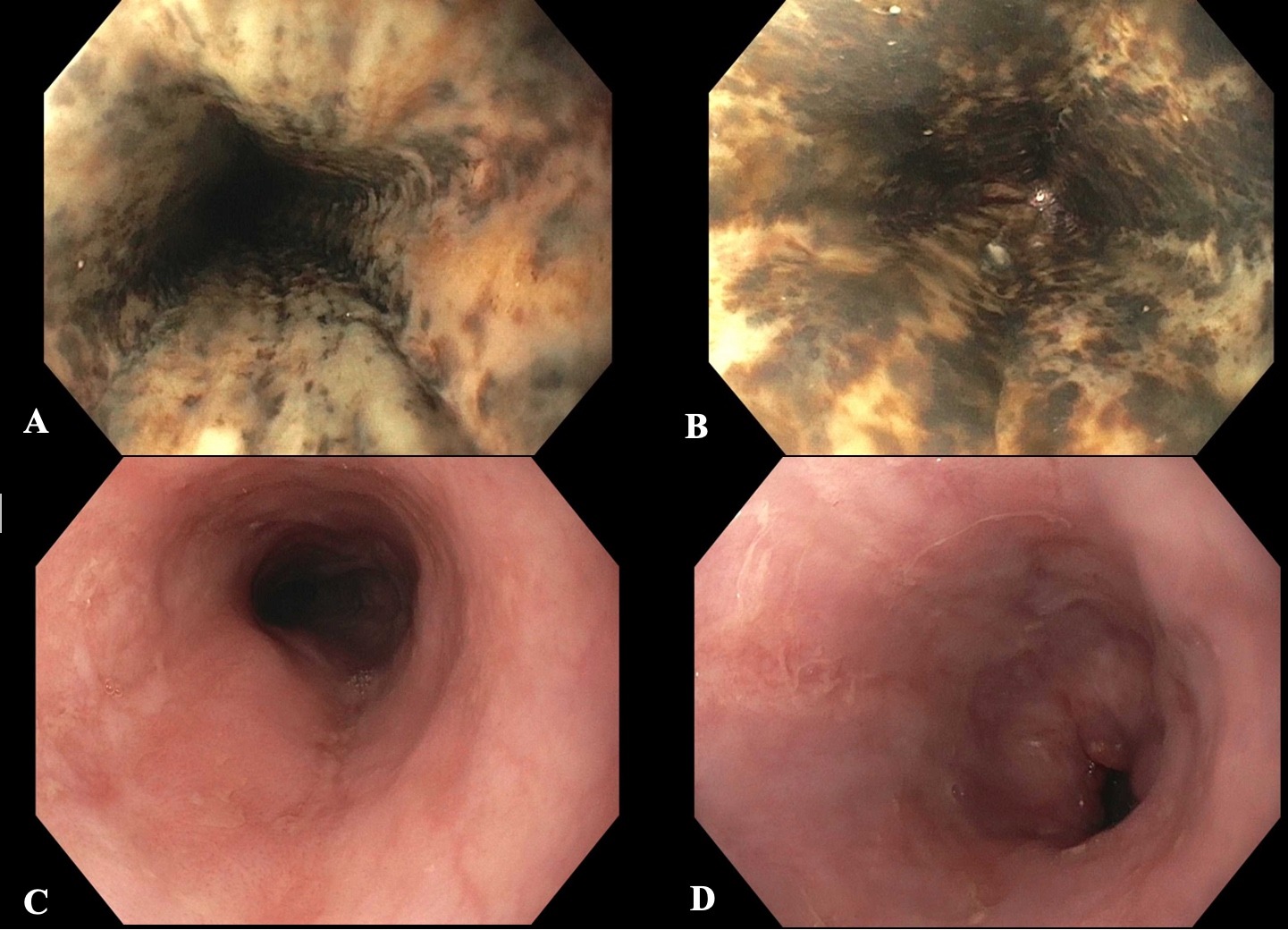
Case Description/Methods: A 77-year-old man presented to the emergency room with post-prandial, epigastric pain. He was hemodynamically stable on presentation. A CT scan of the abdomen demonstrated cholecystitis with a dilated common bile duct (CBD) up to 10mm. Due to concerns for biliary obstruction, a magnetic resonance cholangiopancreatography (MRCP) was done and showed a hypointense filling defect within the cystic duct and CBD. The patient underwent cholecystectomy with removal of a necrotic gallbladder. An intraoperative cholangiogram showed stones that could not be flushed, but CBD exploration was deferred due to friability of the surrounding tissue. The procedure was also complicated by hypotension, requiring 15 minutes of phenylephrine infusion and hypoxia which resolved with a non-rebreather mask. The next day, an esophagogastroduodenoscopy (EGD) and endoscopic ultrasound (EUS) was done to evaluate for any retained stones. The EGD was notable for Los Angeles (LA) Grade D esophagitis with black pigmentation of the esophagus starting 20cm from the incisors down to the gastroesophageal junction (Figure A and B). There were also small, nonbleeding erosions seen in the duodenal bulb and second portion of the duodenum. No choledocholithiasis was seen on EUS. Biopsies of the esophagus showed necrotic tissue with fibrinopurulent debris, confirming the diagnosis of AEN. The patient was started on an oral, high-dose proton pump inhibitor twice daily for management. Repeat EGD performed 11 weeks later demonstrated only residual LA Grade B esophagitis (Figure C and D).
Discussion: AEN has been associated with ischemic injuries, trauma, vasculopathy, sepsis, and general hemodynamic instability. Prognosis can be poor, but early recognition and aggressive supportive care can improve outcomes. This patient developed AEN following a transient period of intraoperative hypotension. Despite the degree of esophageal involvement, this patient lacked any symptoms of dyspepsia or reflux. Therefore, in patients with risk factors for AEN, performing an EGD prior to EUS should be considered even if there is no clinical evidence of hematemesis.
Disclosures:
Jacqueline P. Chang, MD, Eric R. Yoo, MD, Jessica Yu, MD, MS. D0237 - Incidental Acute Esophageal Necrosis in a Post-Cholecystectomy Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Oregon Health & Science University, Portland, OR
Introduction: Acute esophageal necrosis (AEN), or “black esophagus”, is a rare clinical entity characterized by diffuse, black mucosal discoloration of the esophagus on endoscopy. Patients often present with hematemesis, shock, and melena. The condition has a relatively high mortality rate due to the comorbid conditions that are frequently present at the time of diagnosis.
Case Description/Methods: A 77-year-old man presented to the emergency room with post-prandial, epigastric pain. He was hemodynamically stable on presentation. A CT scan of the abdomen demonstrated cholecystitis with a dilated common bile duct (CBD) up to 10mm. Due to concerns for biliary obstruction, a magnetic resonance cholangiopancreatography (MRCP) was done and showed a hypointense filling defect within the cystic duct and CBD. The patient underwent cholecystectomy with removal of a necrotic gallbladder. An intraoperative cholangiogram showed stones that could not be flushed, but CBD exploration was deferred due to friability of the surrounding tissue. The procedure was also complicated by hypotension, requiring 15 minutes of phenylephrine infusion and hypoxia which resolved with a non-rebreather mask. The next day, an esophagogastroduodenoscopy (EGD) and endoscopic ultrasound (EUS) was done to evaluate for any retained stones. The EGD was notable for Los Angeles (LA) Grade D esophagitis with black pigmentation of the esophagus starting 20cm from the incisors down to the gastroesophageal junction (Figure A and B). There were also small, nonbleeding erosions seen in the duodenal bulb and second portion of the duodenum. No choledocholithiasis was seen on EUS. Biopsies of the esophagus showed necrotic tissue with fibrinopurulent debris, confirming the diagnosis of AEN. The patient was started on an oral, high-dose proton pump inhibitor twice daily for management. Repeat EGD performed 11 weeks later demonstrated only residual LA Grade B esophagitis (Figure C and D).
Discussion: AEN has been associated with ischemic injuries, trauma, vasculopathy, sepsis, and general hemodynamic instability. Prognosis can be poor, but early recognition and aggressive supportive care can improve outcomes. This patient developed AEN following a transient period of intraoperative hypotension. Despite the degree of esophageal involvement, this patient lacked any symptoms of dyspepsia or reflux. Therefore, in patients with risk factors for AEN, performing an EGD prior to EUS should be considered even if there is no clinical evidence of hematemesis.
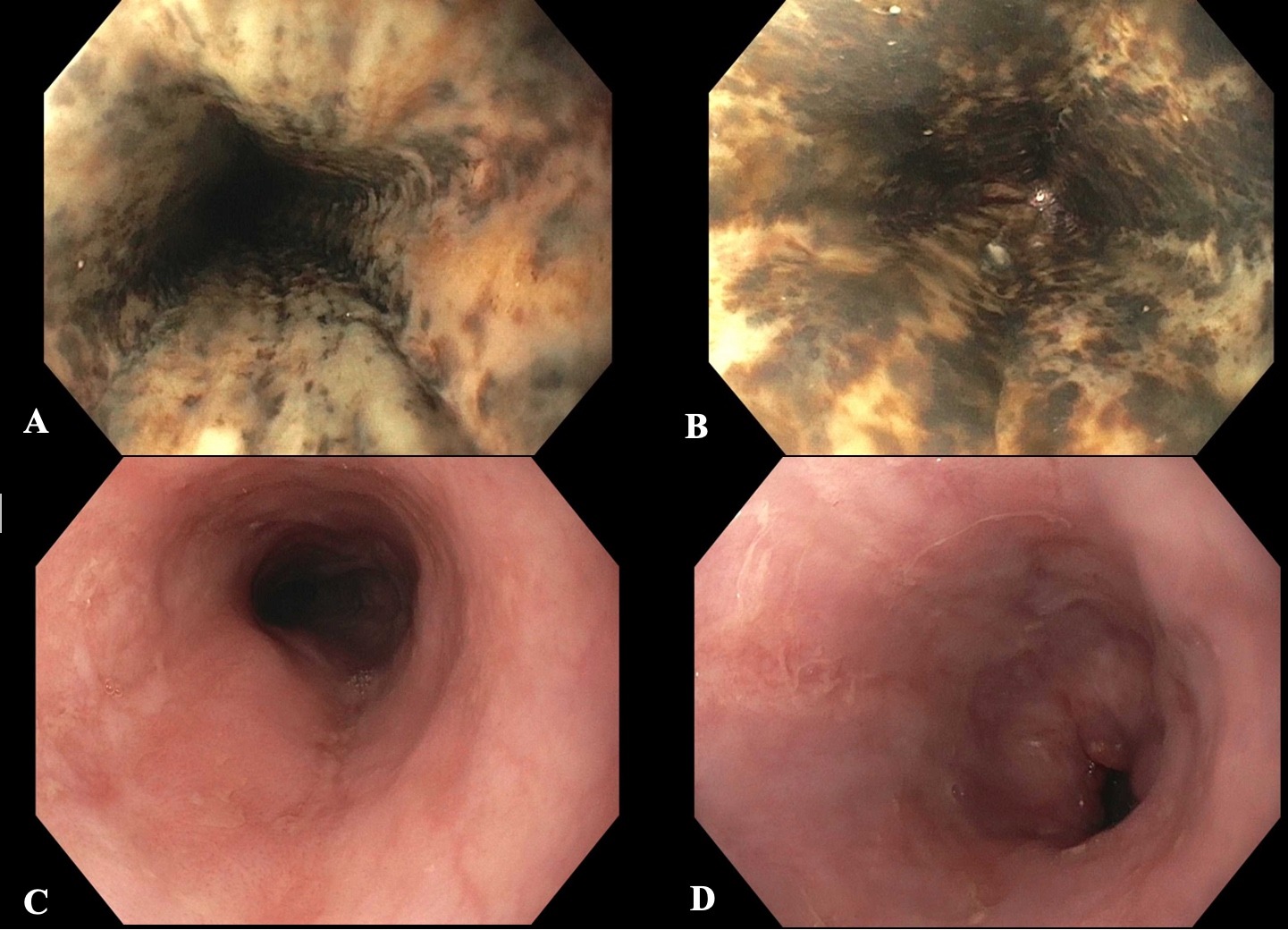
Figure: Endoscopic images of the middle and distal esophagus demonstrating acute esophageal necrosis (A, B). Follow-up EGD 11 weeks later showed resolution of black pigmentation following high-dose PPI treatment (C, D).
Disclosures:
Jacqueline Chang indicated no relevant financial relationships.
Eric Yoo indicated no relevant financial relationships.
Jessica Yu indicated no relevant financial relationships.
Jacqueline P. Chang, MD, Eric R. Yoo, MD, Jessica Yu, MD, MS. D0237 - Incidental Acute Esophageal Necrosis in a Post-Cholecystectomy Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

