Back

Poster Session D - Tuesday Morning
Category: IBD
D0393 - Assessment of Inflammatory Bowel Disease Training Among Gastroenterology Fellows
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Badr Al Bawardy, MD
Yale University School of Medicine
New Haven, CT
Presenting Author(s)
Badr Al-Bawardy, MD1, Lisa Malter, MD2, Adam C. Ehrlich, MD, MPH3, Florian Rieder, MD4, Jill K. Gaidos, MD1, Deborah Proctor, MD1, Donna Windish, MD, MPH1
1Yale University School of Medicine, New Haven, CT; 2NYU/Bellevue, New York, NY; 3Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 4Lerner Research Institute, Cleveland Clinic Foundation, Cleveland, OH
Introduction: The management of inflammatory bowel disease (IBD) is rapidly changing with the expansion of approved therapeutic agents and evolving treatment paradigms. We aimed to assess confidence and training in IBD among gastroenterology (GI) fellows
Methods: This was a multicenter survey study of US GI fellows from December 2021-April 2022. The survey was voluntary, anonymous, and distributed electronically. The survey evaluated fellows’ confidence level in IBD management (scale of 1-4; 1: not confident at all, 4: extremely confident), methods of IBD training received, and amount of additional training desired [None, A little (1 hour), A Moderate Amount (2-3 hours), A Lot ( >3 hours)] in 20 core IBD domains. GI fellows’ preferred learning method was evaluated.
Results: A total of 113 of 175 fellows (65%) from 17 GI fellowship programs responded to the survey. The respondents were distributed evenly between first, second and third year fellows (36.8% 28.7%, 33.3% respectively). Most fellows (85%) were training at academic institutions (55.2% had an IBD center).
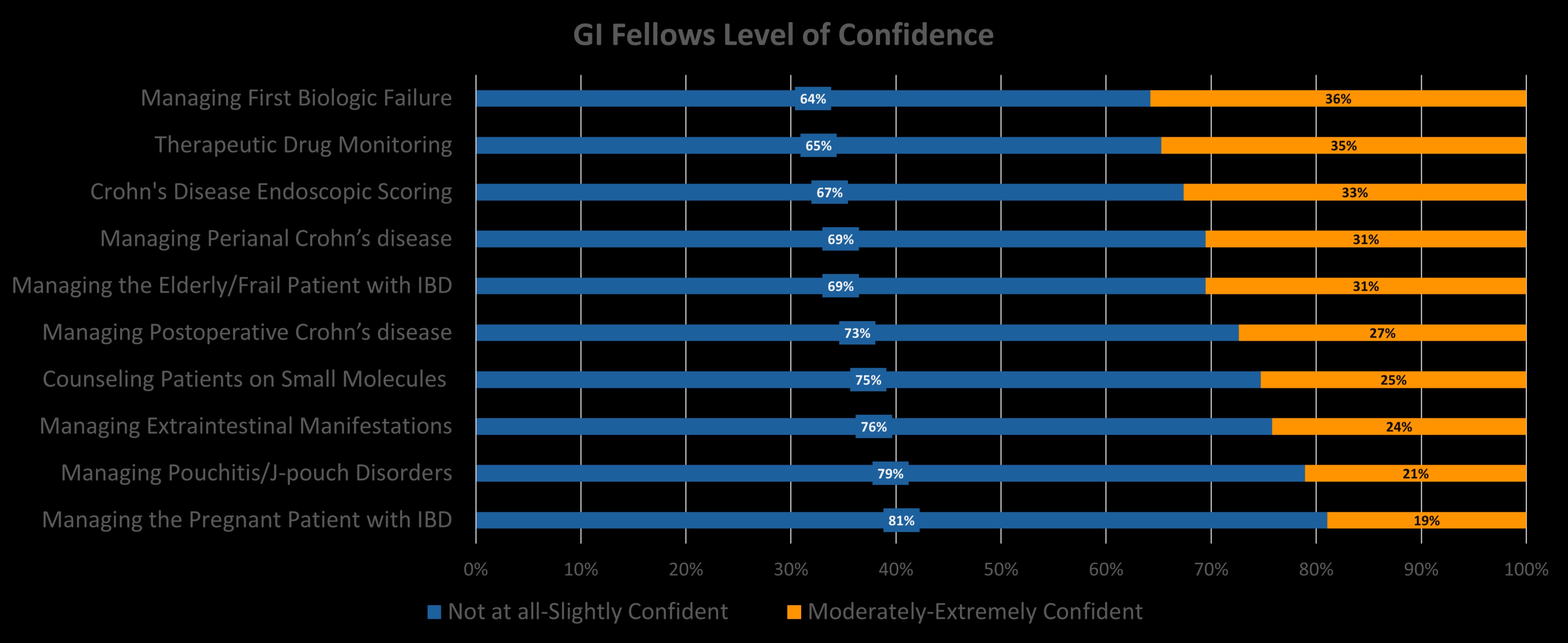
Confidence rating was low (not at all-to-slightly confident) in managing the pregnant patient with IBD (81.1%) followed by managing pouch disorders (78.9%) (Figure). Confidence scores were highest in managing the hospitalized patient with ulcerative colitis (82.1% moderately-extremely confident). More than 50% of 3rd year fellows reported low confidence in managing the pregnant patient, pouch disorders, extraintestinal manifestations (EIMs), postoperative Crohn’s disease (CD) and counseling patients on small molecules.
Fellows reported receiving no IBD specific training in managing the elderly patient (23.0%), EIMs (12.6%) and diet/nutrition counseling (12.5%).
Most fellows (64.4%-68.9%) desired a moderate to a lot more training (≥ 2 hours) in: therapeutic drug monitoring, managing the patient with IBD failing first line biologic therapy, counseling patients on biologics/small molecules, managing the elderly patient, perianal CD, EIMs and pouch disorders. Recorded web-based lecture was ranked as the number one preferred learning strategy by 25.7% followed by live case-based lecture (23%) and live didactic lecture (23%).
Discussion: Most GI fellows lacked confidence and training in key domains of IBD management. This may result in significant implications on the quality of IBD care. A focused and sustainable curriculum for GI fellows addressing the identified gaps of knowledge in IBD management is warranted.
Disclosures:
Badr Al-Bawardy, MD1, Lisa Malter, MD2, Adam C. Ehrlich, MD, MPH3, Florian Rieder, MD4, Jill K. Gaidos, MD1, Deborah Proctor, MD1, Donna Windish, MD, MPH1. D0393 - Assessment of Inflammatory Bowel Disease Training Among Gastroenterology Fellows, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Yale University School of Medicine, New Haven, CT; 2NYU/Bellevue, New York, NY; 3Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 4Lerner Research Institute, Cleveland Clinic Foundation, Cleveland, OH
Introduction: The management of inflammatory bowel disease (IBD) is rapidly changing with the expansion of approved therapeutic agents and evolving treatment paradigms. We aimed to assess confidence and training in IBD among gastroenterology (GI) fellows
Methods: This was a multicenter survey study of US GI fellows from December 2021-April 2022. The survey was voluntary, anonymous, and distributed electronically. The survey evaluated fellows’ confidence level in IBD management (scale of 1-4; 1: not confident at all, 4: extremely confident), methods of IBD training received, and amount of additional training desired [None, A little (1 hour), A Moderate Amount (2-3 hours), A Lot ( >3 hours)] in 20 core IBD domains. GI fellows’ preferred learning method was evaluated.
Results: A total of 113 of 175 fellows (65%) from 17 GI fellowship programs responded to the survey. The respondents were distributed evenly between first, second and third year fellows (36.8% 28.7%, 33.3% respectively). Most fellows (85%) were training at academic institutions (55.2% had an IBD center).
Confidence rating was low (not at all-to-slightly confident) in managing the pregnant patient with IBD (81.1%) followed by managing pouch disorders (78.9%) (Figure). Confidence scores were highest in managing the hospitalized patient with ulcerative colitis (82.1% moderately-extremely confident). More than 50% of 3rd year fellows reported low confidence in managing the pregnant patient, pouch disorders, extraintestinal manifestations (EIMs), postoperative Crohn’s disease (CD) and counseling patients on small molecules.
Fellows reported receiving no IBD specific training in managing the elderly patient (23.0%), EIMs (12.6%) and diet/nutrition counseling (12.5%).
Most fellows (64.4%-68.9%) desired a moderate to a lot more training (≥ 2 hours) in: therapeutic drug monitoring, managing the patient with IBD failing first line biologic therapy, counseling patients on biologics/small molecules, managing the elderly patient, perianal CD, EIMs and pouch disorders. Recorded web-based lecture was ranked as the number one preferred learning strategy by 25.7% followed by live case-based lecture (23%) and live didactic lecture (23%).
Discussion: Most GI fellows lacked confidence and training in key domains of IBD management. This may result in significant implications on the quality of IBD care. A focused and sustainable curriculum for GI fellows addressing the identified gaps of knowledge in IBD management is warranted.
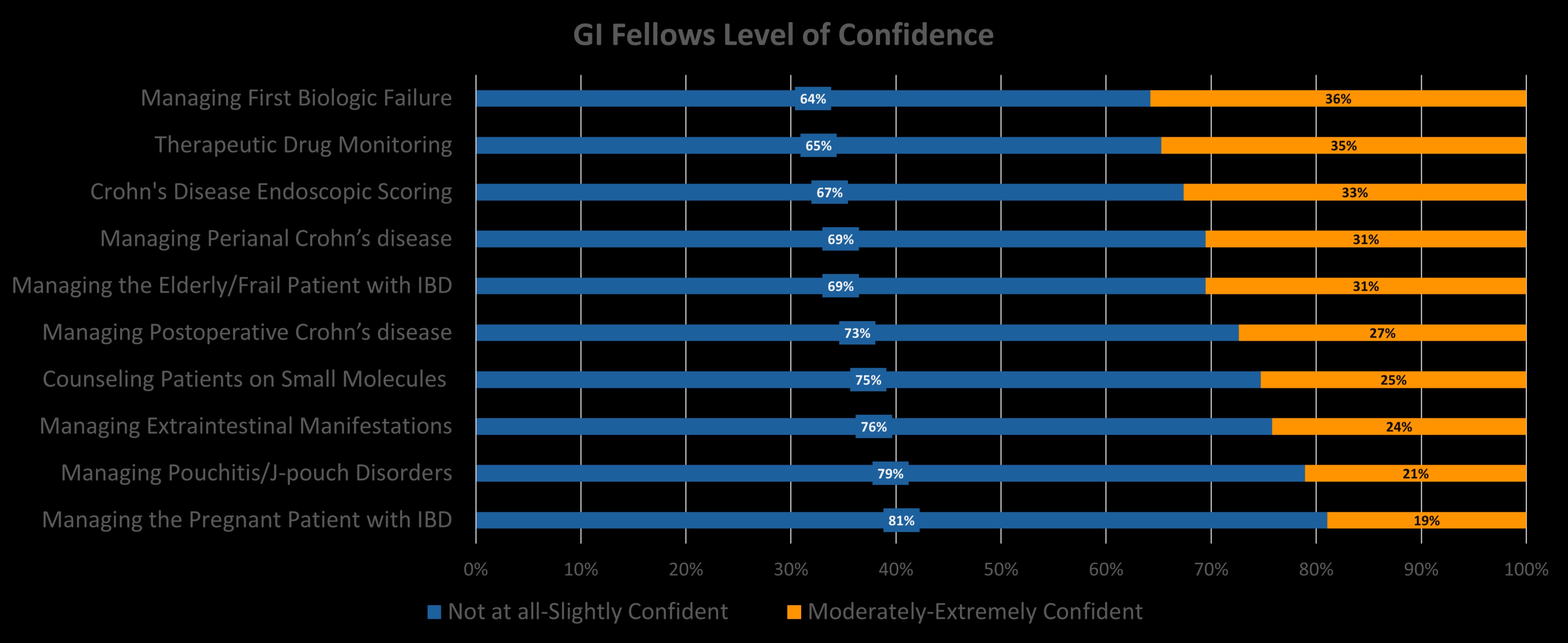
Figure: GI fellows level of confidence in inflammatory bowel disease domains.
Disclosures:
Badr Al-Bawardy: AbbVie – Speakers Bureau. Bristol Myers Squibb – Advisor or Review Panel Member. Takeda – Speakers Bureau.
Lisa Malter: Abbvie – Advisory Committee/Board Member. Abbvie – Grant/Research Support. Gilead – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Janssen – Grant/Research Support. Merck – Advisory Committee/Board Member. Pfizer – Grant/Research Support. Takeda – Advisory Committee/Board Member. Takeda – Grant/Research Support. UCB – Grant/Research Support.
Adam Ehrlich: Bristol Meyers Scquibb – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member.
Florian Rieder: 89Bio – Advisory Committee/Board Member, Consultant. AbbVie – Advisory Committee/Board Member, Consultant. Adnovate – Advisory Committee/Board Member, Consultant. Agomab – Advisory Committee/Board Member, Consultant. Allergan – Advisory Committee/Board Member, Consultant. Arena – Advisory Committee/Board Member, Consultant. Boehringer-Ingelheim – Advisory Committee/Board Member, Consultant. CDISC – Advisory Committee/Board Member, Consultant. Celgene/BMS – Advisory Committee/Board Member, Consultant. Cowen – Advisory Committee/Board Member, Consultant. Ferring – Advisory Committee/Board Member, Consultant. Galapagos – Advisory Committee/Board Member, Consultant. Galmed – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. Gossamer – Advisory Committee/Board Member, Consultant. Guidepoint – Advisory Committee/Board Member, Consultant. Helmsley – Advisory Committee/Board Member, Consultant. Horizon Therapeutics – Advisory Committee/Board Member, Consultant. Image Analysis Limited – Advisory Committee/Board Member, Consultant. Index Pharma – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant. Koutif – Advisory Committee/Board Member, Consultant. Mestag – Advisory Committee/Board Member, Consultant. Metacrine – Advisory Committee/Board Member, Consultant. Morphic – Advisory Committee/Board Member, Consultant. Organovo – Advisory Committee/Board Member, Consultant. Origo – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Pliant – Advisory Committee/Board Member, Consultant. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Receptos – Advisory Committee/Board Member, Consultant. RedX – Advisory Committee/Board Member, Consultant. Roche – Advisory Committee/Board Member, Consultant. Samsung – Advisory Committee/Board Member, Consultant. Surmodics – Advisory Committee/Board Member, Consultant. Surrozen – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant. Techlab – Advisory Committee/Board Member, Consultant. Theravance – Advisory Committee/Board Member, Consultant. Thetis – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant. Ysios – Advisory Committee/Board Member, Consultant.
Jill Gaidos: AbbVie – Speakers Bureau.
Deborah Proctor: AbbVie – Consultant, Grant/Research Support. Celgene – Grant/Research Support. Parexel – Grant/Research Support.
Donna Windish indicated no relevant financial relationships.
Badr Al-Bawardy, MD1, Lisa Malter, MD2, Adam C. Ehrlich, MD, MPH3, Florian Rieder, MD4, Jill K. Gaidos, MD1, Deborah Proctor, MD1, Donna Windish, MD, MPH1. D0393 - Assessment of Inflammatory Bowel Disease Training Among Gastroenterology Fellows, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

