Back

Poster Session D - Tuesday Morning
Category: IBD
D0424 - Purpura Fulminans in Acute Severe Ulcerative Colitis Successfully Treated With Infliximab
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Gabriela Kuftinec, MD, MPH
Kaiser Permanente
Los Angeles, CA
Presenting Author(s)
Gabriela Kuftinec, MD, MPH1, Jane Lim, MD1, Phillip Gu, MD2, Andres Yarur, MD3
1Kaiser Permanente, Los Angeles, CA; 2Cedars Sinai Medical Center, Los Angeles, CA; 3Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Several extra-intestinal dermatological manifestations can be seen in patients with ulcerative colitis (UC). We report a rare case of purpura fulminans in the setting of acute, severe UC (ASUC). A few reports have shown improvement of this entity only with colectomy. We describe a case of purpura fulminans that developed in the setting of ASUC that responded with infliximab (IFX) therapy.
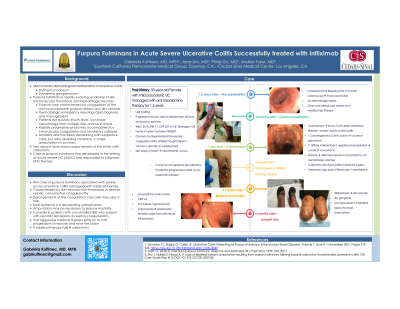
Case Description/Methods: A 50-year-old Female with mild pan-UC and no previous dermatologic morbidity managed with oral mesalamine therapy for 18 months developed exacerbation of symptoms. Colonoscopy reveled moderate pancolitis (Endoscopic Mayo 2). She was started on prednisone and vedolizumab but after a partial response, lost response and developed worsening gastrointestinal (GI) symptoms and presented with vesiculated, hemorrhagic bullae involving both feet, left arm and back (Figure 1A). White blood cell count on admission was 35,700, International normalized ratio (INR) 1.7, C-reaction protein (CRP) 227 mg/L and fibrinogen 129 (mg/dl). Skin biopsy showed microthrombi but no pus. Patient was started on corticosteroids, with mild improvement in GI symptoms but worsening skin lesions. Given case reports of purpura fulminans resolving with colectomy, the procedure was offered but declined by the patient. She was started on IFX (10 mg/Kg). Her GI symptoms improved and her skin lesions stabilized. After discharge, the skin lesions on her back and arm healed, but both feet developed skin necrosis and dry gangrene, requiring a bilateral below the knee amputations (Figure 1B). After 14 weeks of IFX therapy, the patient is in clinical remission, normalized CRP and only with a limited area of mucosal inflammation in the sigmoid on colonoscopy.
Discussion: To our knowledge, this is the first case of purpura fulminans in association with ASUC that responded to infliximab. While the patient required amputation, therapy with infliximab slowed the progression of her disease, limiting the areas of necrosis and potentially avoiding sepsis. Pupura fulminans is characterized by skin necrosis with thrombosis in the dermal vessels and consumptive coagulopathy. Limb ischemia is a devastating complication and amputation may be necessary to reduce mortality. In conclusion, patients with ASUC that develop purpura fulminans may benefit of early and aggressive medical therapy with IFX, sparing the need for colectomy.

Disclosures:
Gabriela Kuftinec, MD, MPH1, Jane Lim, MD1, Phillip Gu, MD2, Andres Yarur, MD3. D0424 - Purpura Fulminans in Acute Severe Ulcerative Colitis Successfully Treated With Infliximab, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Kaiser Permanente, Los Angeles, CA; 2Cedars Sinai Medical Center, Los Angeles, CA; 3Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Several extra-intestinal dermatological manifestations can be seen in patients with ulcerative colitis (UC). We report a rare case of purpura fulminans in the setting of acute, severe UC (ASUC). A few reports have shown improvement of this entity only with colectomy. We describe a case of purpura fulminans that developed in the setting of ASUC that responded with infliximab (IFX) therapy.
Case Description/Methods: A 50-year-old Female with mild pan-UC and no previous dermatologic morbidity managed with oral mesalamine therapy for 18 months developed exacerbation of symptoms. Colonoscopy reveled moderate pancolitis (Endoscopic Mayo 2). She was started on prednisone and vedolizumab but after a partial response, lost response and developed worsening gastrointestinal (GI) symptoms and presented with vesiculated, hemorrhagic bullae involving both feet, left arm and back (Figure 1A). White blood cell count on admission was 35,700, International normalized ratio (INR) 1.7, C-reaction protein (CRP) 227 mg/L and fibrinogen 129 (mg/dl). Skin biopsy showed microthrombi but no pus. Patient was started on corticosteroids, with mild improvement in GI symptoms but worsening skin lesions. Given case reports of purpura fulminans resolving with colectomy, the procedure was offered but declined by the patient. She was started on IFX (10 mg/Kg). Her GI symptoms improved and her skin lesions stabilized. After discharge, the skin lesions on her back and arm healed, but both feet developed skin necrosis and dry gangrene, requiring a bilateral below the knee amputations (Figure 1B). After 14 weeks of IFX therapy, the patient is in clinical remission, normalized CRP and only with a limited area of mucosal inflammation in the sigmoid on colonoscopy.
Discussion: To our knowledge, this is the first case of purpura fulminans in association with ASUC that responded to infliximab. While the patient required amputation, therapy with infliximab slowed the progression of her disease, limiting the areas of necrosis and potentially avoiding sepsis. Pupura fulminans is characterized by skin necrosis with thrombosis in the dermal vessels and consumptive coagulopathy. Limb ischemia is a devastating complication and amputation may be necessary to reduce mortality. In conclusion, patients with ASUC that develop purpura fulminans may benefit of early and aggressive medical therapy with IFX, sparing the need for colectomy.

Figure: Purpura fulminant at presentation and follow-up
Disclosures:
Gabriela Kuftinec indicated no relevant financial relationships.
Jane Lim indicated no relevant financial relationships.
Phillip Gu indicated no relevant financial relationships.
Andres Yarur: Arena Pharmaceuticals – Consultant. Bristol Myers Squibb – Consultant. Prometheus Laboratories – Consultant. Takeda – Advisory Committee/Board Member.
Gabriela Kuftinec, MD, MPH1, Jane Lim, MD1, Phillip Gu, MD2, Andres Yarur, MD3. D0424 - Purpura Fulminans in Acute Severe Ulcerative Colitis Successfully Treated With Infliximab, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

