Back

Poster Session C - Monday Afternoon
Category: Liver
C0495 - Trends and Disparities in Outcomes of Hospitalizations With Portal Vein Thrombosis: Analysis of the Nationwide Inpatient Sample
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
Robert Kwei-Nsoro, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Robert Kwei-Nsoro, MD1, Pius E. Ojemolon, MD1, Adewale Adedoyin, MBBS2, Hisham Laswi, MD1, Ebehiwele Ebhohon, MD3, Katayoun Khoshbin, MD1, Hafeez Shaka, MBBS1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Englewood Hospital, Englewood, NJ; 3Lincoln Medical Center, Bronx, NY
Introduction: Portal vein thrombosis is a relatively rare disease, it is however becoming increasingly recognized in developed countries.Reliable data on epidemiological trends and outcomes of hospitalization is lacking. This study aimed to describe the epidemiological trends and the sociodemographic factors that affect outcomes of PVT hospitalization.
Methods: This was a retrospective longitudinal study involving hospitalizations with portal vein thrombosis (PVT) in the US from 2010 to 2019. We sourced data from the Nationwide Inpatient Sample databases from 2010 through to 2019. The study involved two cohorts of hospitalizations; any hospitalization with PVT, and hospitalizations with a principal discharge diagnosis of PVT.We calculated the admission rate and the incidence of PVT per million adult hospitalizations during each calendar year. We used multivariable regression trend analysis to obtain trends in mortality, length of stay (LOS), and total hospital charges (THC) adjusted for age categories, sex, and race.
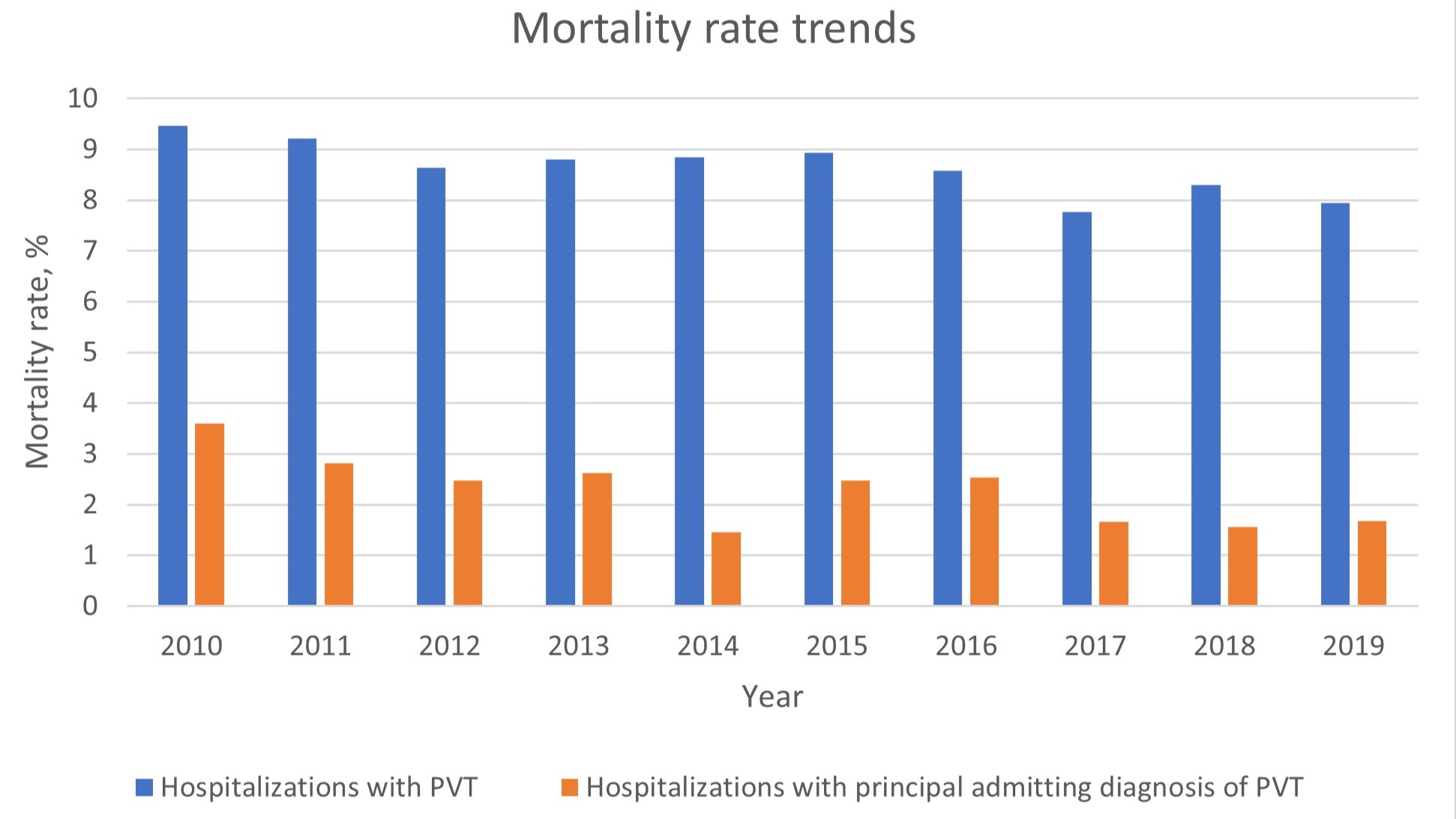
Results: The adjusted incidence rate of PVT per million hospitalizations increased from 666 in 2010 to 1898 in 2019, with an annual percentage change (APC) of 13.8% (p < 0.001). PVT admission rate per million hospitalizations increased from 68 in 2010, to 189 in 2019, with an average APC of 14.8% (p < 0.001).There was a statistically significant reduction in trends of mortality rate from 9.5% to 7.9% over the decade (p 0.017). We also noticed a gradual decline in LOS, from 9.2 days in 2010 to 8.0 days in 2019.There was a significant uptrend in the mean THC over the decade from 99,626$ to 109,558$.Multivariate analysis showed that middle-aged and the elderly compared to young patients were more likely to have higher mortality rates. There was no significant difference observed in mortality rates, LOS and THC when both genders were compared.Blacks had a 30% higher odds of mortality over the period compared to Whites (p < 0.001). The THC was significantly higher in Hispanics compared to Whites (p < 0.001).
Discussion: While the crude incidence rate significantly increased over the years, we also noticed a gradual decline in the mortality rates over the same period; this observation is likely due to the advancements in the diagnosis and management of PVT over the decade. The middle-aged, elderly, Black and Hispanic populations are often associated with adverse outcomes during hospitalization for PVT.Additional studies are needed to further explore these findings.
Disclosures:
Robert Kwei-Nsoro, MD1, Pius E. Ojemolon, MD1, Adewale Adedoyin, MBBS2, Hisham Laswi, MD1, Ebehiwele Ebhohon, MD3, Katayoun Khoshbin, MD1, Hafeez Shaka, MBBS1. C0495 - Trends and Disparities in Outcomes of Hospitalizations With Portal Vein Thrombosis: Analysis of the Nationwide Inpatient Sample, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Englewood Hospital, Englewood, NJ; 3Lincoln Medical Center, Bronx, NY
Introduction: Portal vein thrombosis is a relatively rare disease, it is however becoming increasingly recognized in developed countries.Reliable data on epidemiological trends and outcomes of hospitalization is lacking. This study aimed to describe the epidemiological trends and the sociodemographic factors that affect outcomes of PVT hospitalization.
Methods: This was a retrospective longitudinal study involving hospitalizations with portal vein thrombosis (PVT) in the US from 2010 to 2019. We sourced data from the Nationwide Inpatient Sample databases from 2010 through to 2019. The study involved two cohorts of hospitalizations; any hospitalization with PVT, and hospitalizations with a principal discharge diagnosis of PVT.We calculated the admission rate and the incidence of PVT per million adult hospitalizations during each calendar year. We used multivariable regression trend analysis to obtain trends in mortality, length of stay (LOS), and total hospital charges (THC) adjusted for age categories, sex, and race.
Results: The adjusted incidence rate of PVT per million hospitalizations increased from 666 in 2010 to 1898 in 2019, with an annual percentage change (APC) of 13.8% (p < 0.001). PVT admission rate per million hospitalizations increased from 68 in 2010, to 189 in 2019, with an average APC of 14.8% (p < 0.001).There was a statistically significant reduction in trends of mortality rate from 9.5% to 7.9% over the decade (p 0.017). We also noticed a gradual decline in LOS, from 9.2 days in 2010 to 8.0 days in 2019.There was a significant uptrend in the mean THC over the decade from 99,626$ to 109,558$.Multivariate analysis showed that middle-aged and the elderly compared to young patients were more likely to have higher mortality rates. There was no significant difference observed in mortality rates, LOS and THC when both genders were compared.Blacks had a 30% higher odds of mortality over the period compared to Whites (p < 0.001). The THC was significantly higher in Hispanics compared to Whites (p < 0.001).
Discussion: While the crude incidence rate significantly increased over the years, we also noticed a gradual decline in the mortality rates over the same period; this observation is likely due to the advancements in the diagnosis and management of PVT over the decade. The middle-aged, elderly, Black and Hispanic populations are often associated with adverse outcomes during hospitalization for PVT.Additional studies are needed to further explore these findings.
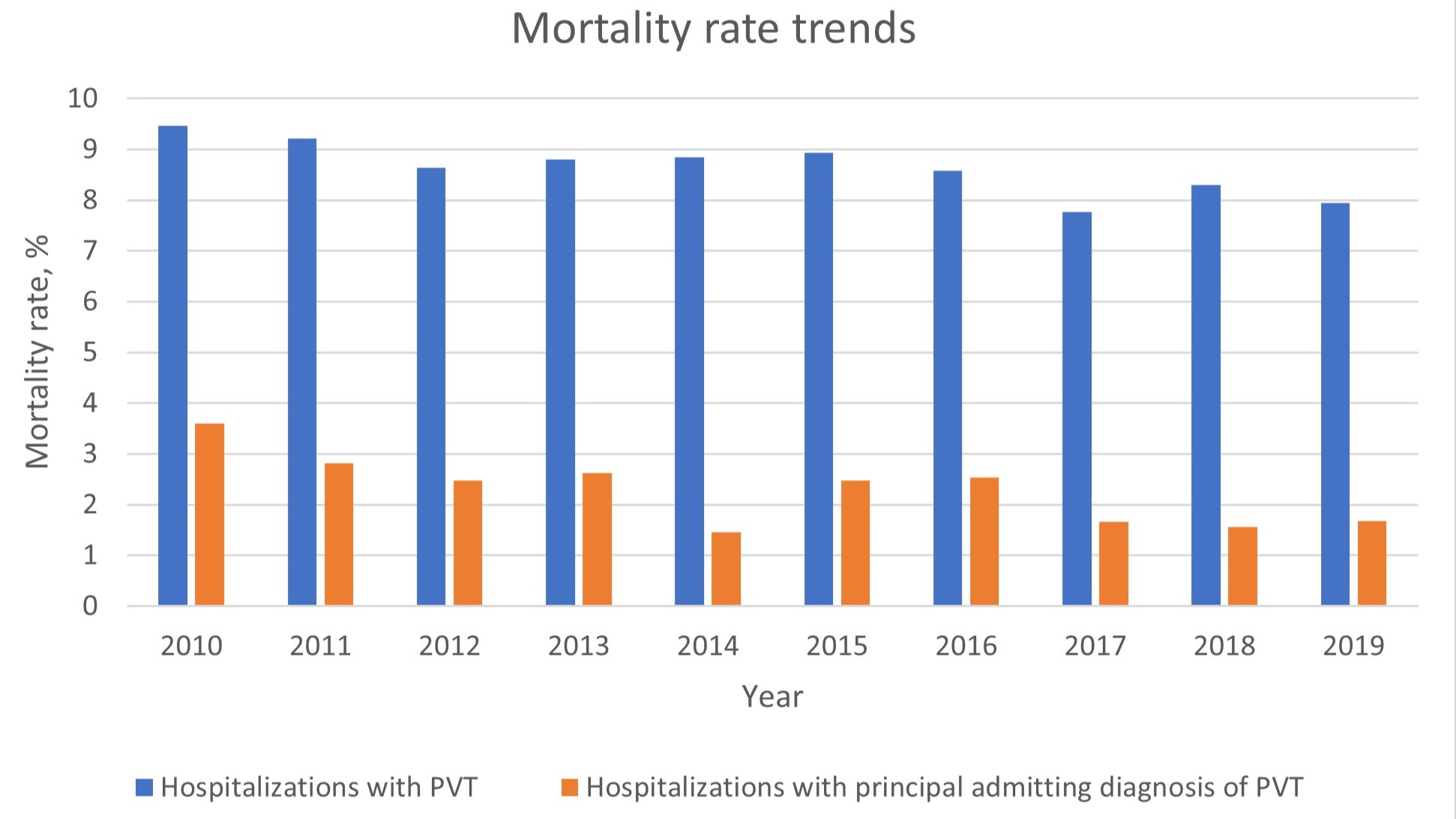
Figure: Trends in mortality rates among total hospitalizations with PVT and admissions with PVT as principal diagnosis.
Disclosures:
Robert Kwei-Nsoro indicated no relevant financial relationships.
Pius Ojemolon indicated no relevant financial relationships.
Adewale Adedoyin indicated no relevant financial relationships.
Hisham Laswi indicated no relevant financial relationships.
Ebehiwele Ebhohon indicated no relevant financial relationships.
Katayoun Khoshbin indicated no relevant financial relationships.
Hafeez Shaka indicated no relevant financial relationships.
Robert Kwei-Nsoro, MD1, Pius E. Ojemolon, MD1, Adewale Adedoyin, MBBS2, Hisham Laswi, MD1, Ebehiwele Ebhohon, MD3, Katayoun Khoshbin, MD1, Hafeez Shaka, MBBS1. C0495 - Trends and Disparities in Outcomes of Hospitalizations With Portal Vein Thrombosis: Analysis of the Nationwide Inpatient Sample, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
