Back

Poster Session C - Monday Afternoon
Category: General Endoscopy
C0313 - Post-Transplant Lymphoproliferative Disorder Presenting as Iron Deficiency Anemia: A Case Report
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
Marcella Pimpinelli, MD
Rutgers Robert Wood Johnson University Hospital- New Brunswick
New Brunswick, New Jersey
Presenting Author(s)
Marcella Pimpinelli, MD, Peter Dellatore, MD, Abhishek Bhurwal, MD, Mahmoud A. Ali, MBBCh, Anish Vinit Patel, MD
Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Post- Transplant Lymphoproliferative Disease (PTLD) is a rare but well-known complication of transplant recipients on immunosuppression. Even less common is monomorphic B cell type PTLD in a patient negative for the Epstein Barr Virus. Its presentation is highly variable and associated with poor outcomes with later detection.
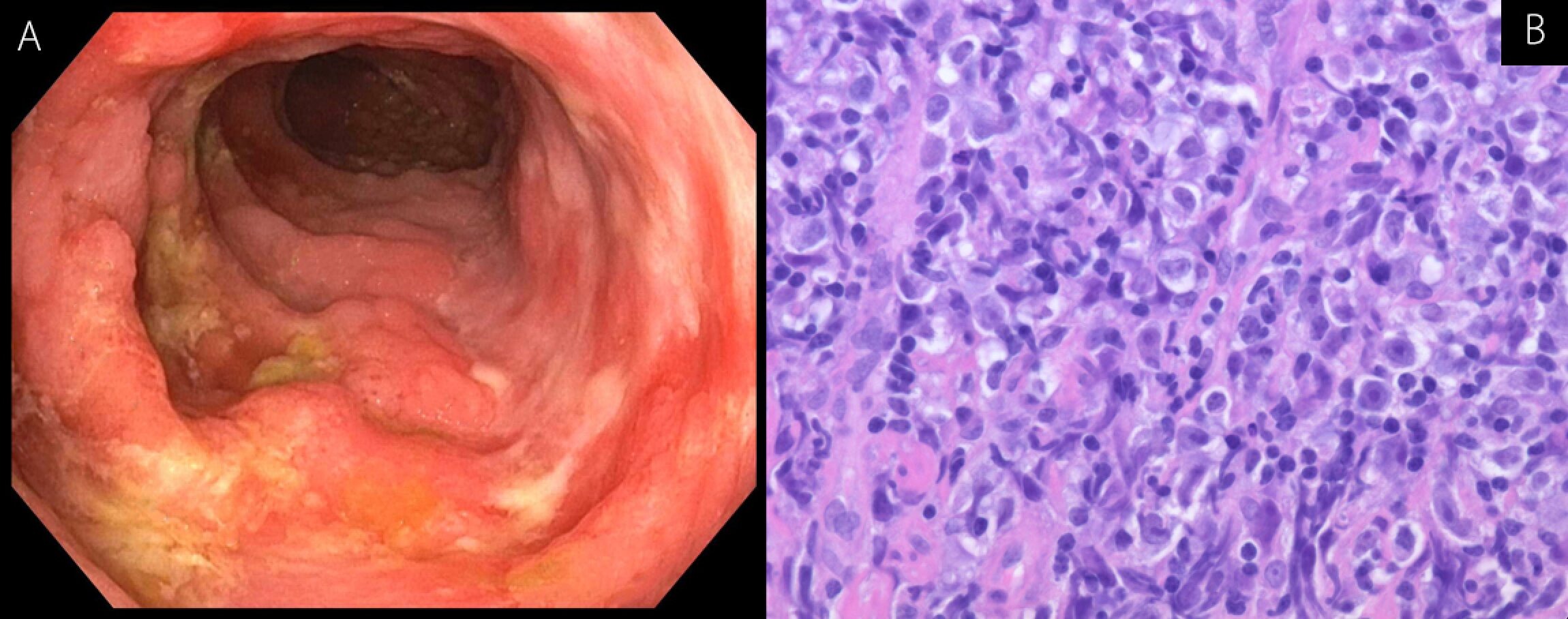
Case Description/Methods: A 29-year-old male presented with nausea, vomiting, fatigue, and 10-pound unintentional weight loss over several weeks. He had a past medical history of congenital solitary kidney, Focal Segmental Glomerular Sclerosis and underwent deceased donor renal transplant 13 years ago. He had remained on chronic immunosuppression (Mycophenolate, tacrolimus, prednisone). His exam was notable only for conjunctival pallor. Labs revealed WBC 10.8 (15% lymphocytes), anemia (Hgb 5.7), iron saturation 6% and thrombocytosis (platelets 1154). Contrast enhanced CT Abdomen and Pelvis revealed necrotic mesenteric lymphadenopathy and thickened small bowel loops in the left hemiabdomen. Upper endoscopy was normal. Colonoscopy exposed an ulcerated lesion with nodular mucosa in the terminal ileum (Fig 1A). Biopsy revealed monomorphic PTLD Diffuse Large B Cell Lymphoma (DLBCL) with CD20 and CD30 expression (Fig 1B). EBV and CMV staining were negative. Further workup with bone marrow biopsy showed no evidence of leukemia or lymphoma. FISH showed trisomy of chromosome 8, 14, and 18, but no bcl2-IgH fusion translocation or C-MYC translocation. He was treated with weekly Rituximab/Ruxience biosimilar followed by the CHOP chemotherapy regimen. However, surveillance imaging showed increase in size of lymph nodes. He continued to deteriorate over the next 3 months and died thereafter.
Discussion: Transplant recipients are vulnerable to PTLD, with greater than 85% of cases of PTLD occurring in the first-year post-transplant. In our case, we described an aggressive course of B cell type monomorphic PTLD 13 years post-transplant in an EBV seronegative patient on chronic immunosuppressants. Most patients are treated with Rituximab and/or CHOP chemotherapy, however, patients with solid organ transplants often do not tolerate such aggressive treatment. New treatments with low toxicity are needed to further improve outcomes for patients with PTLD. Our case also highlights the importance of adequate small bowel evaluation with terminal ileum intubation during colonoscopy and further advanced imaging if necessary for workup of iron deficiency anemia.
Disclosures:
Marcella Pimpinelli, MD, Peter Dellatore, MD, Abhishek Bhurwal, MD, Mahmoud A. Ali, MBBCh, Anish Vinit Patel, MD. C0313 - Post-Transplant Lymphoproliferative Disorder Presenting as Iron Deficiency Anemia: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Post- Transplant Lymphoproliferative Disease (PTLD) is a rare but well-known complication of transplant recipients on immunosuppression. Even less common is monomorphic B cell type PTLD in a patient negative for the Epstein Barr Virus. Its presentation is highly variable and associated with poor outcomes with later detection.
Case Description/Methods: A 29-year-old male presented with nausea, vomiting, fatigue, and 10-pound unintentional weight loss over several weeks. He had a past medical history of congenital solitary kidney, Focal Segmental Glomerular Sclerosis and underwent deceased donor renal transplant 13 years ago. He had remained on chronic immunosuppression (Mycophenolate, tacrolimus, prednisone). His exam was notable only for conjunctival pallor. Labs revealed WBC 10.8 (15% lymphocytes), anemia (Hgb 5.7), iron saturation 6% and thrombocytosis (platelets 1154). Contrast enhanced CT Abdomen and Pelvis revealed necrotic mesenteric lymphadenopathy and thickened small bowel loops in the left hemiabdomen. Upper endoscopy was normal. Colonoscopy exposed an ulcerated lesion with nodular mucosa in the terminal ileum (Fig 1A). Biopsy revealed monomorphic PTLD Diffuse Large B Cell Lymphoma (DLBCL) with CD20 and CD30 expression (Fig 1B). EBV and CMV staining were negative. Further workup with bone marrow biopsy showed no evidence of leukemia or lymphoma. FISH showed trisomy of chromosome 8, 14, and 18, but no bcl2-IgH fusion translocation or C-MYC translocation. He was treated with weekly Rituximab/Ruxience biosimilar followed by the CHOP chemotherapy regimen. However, surveillance imaging showed increase in size of lymph nodes. He continued to deteriorate over the next 3 months and died thereafter.
Discussion: Transplant recipients are vulnerable to PTLD, with greater than 85% of cases of PTLD occurring in the first-year post-transplant. In our case, we described an aggressive course of B cell type monomorphic PTLD 13 years post-transplant in an EBV seronegative patient on chronic immunosuppressants. Most patients are treated with Rituximab and/or CHOP chemotherapy, however, patients with solid organ transplants often do not tolerate such aggressive treatment. New treatments with low toxicity are needed to further improve outcomes for patients with PTLD. Our case also highlights the importance of adequate small bowel evaluation with terminal ileum intubation during colonoscopy and further advanced imaging if necessary for workup of iron deficiency anemia.
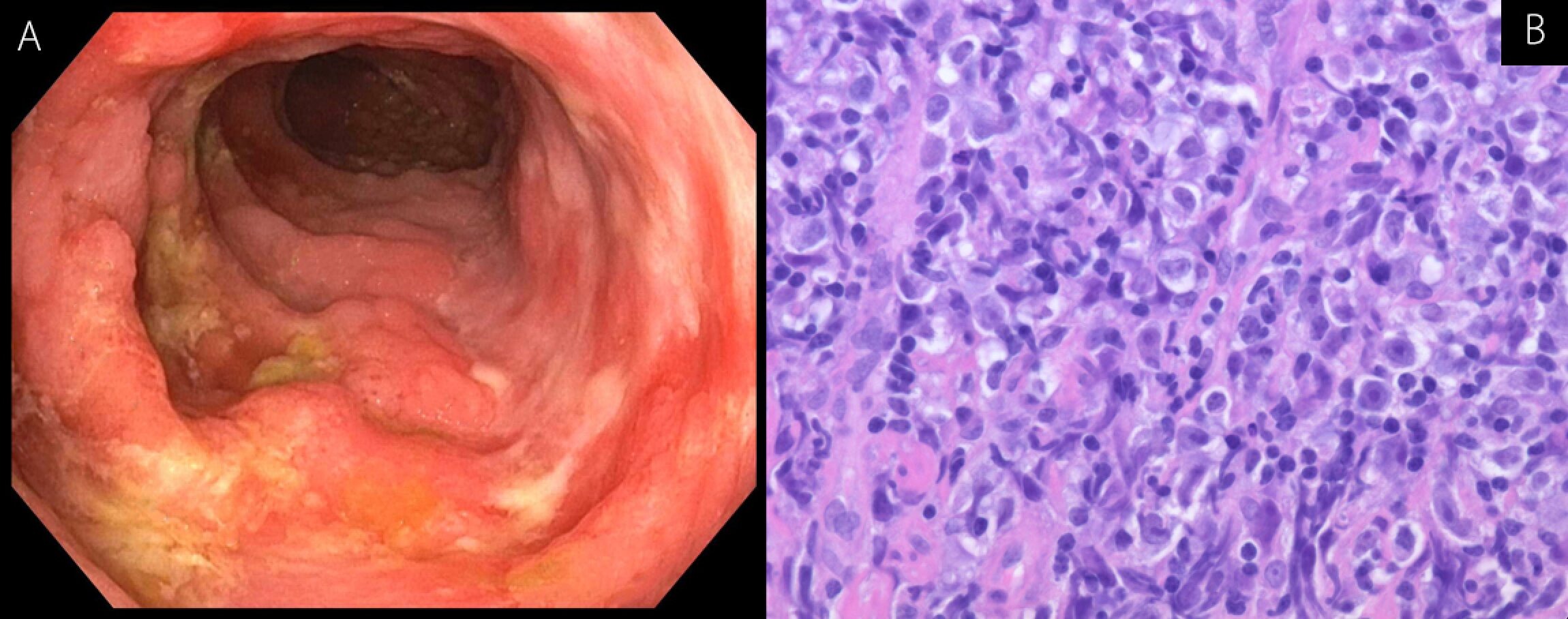
Figure: (Fig. 1A) ulcerated lesion with nodular mucosa in the terminal ileum
(Fig. 1B) histology slide showing monomorphic PTLD Diffuse Large B Cell Lymphoma (DLBCL)
(Fig. 1B) histology slide showing monomorphic PTLD Diffuse Large B Cell Lymphoma (DLBCL)
Disclosures:
Marcella Pimpinelli indicated no relevant financial relationships.
Peter Dellatore indicated no relevant financial relationships.
Abhishek Bhurwal indicated no relevant financial relationships.
Mahmoud Ali indicated no relevant financial relationships.
Anish Vinit Patel indicated no relevant financial relationships.
Marcella Pimpinelli, MD, Peter Dellatore, MD, Abhishek Bhurwal, MD, Mahmoud A. Ali, MBBCh, Anish Vinit Patel, MD. C0313 - Post-Transplant Lymphoproliferative Disorder Presenting as Iron Deficiency Anemia: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
