Back

Poster Session D - Tuesday Morning
Category: Interventional Endoscopy
D0439 - Transoral Incisionless Fundoplication Is a Safe and Effective Therapeutic Option for Refractory GERD: A 3-Year Retrospective Experience at a Quaternary Center
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Henry Lam, DO
Lehigh Valley Health Network
Allentown, PA
Presenting Author(s)
Henry Lam, DO1, Arjan Ahluwalia, MD1, Michal Kloska, MD, PhD2, Abdul Aleem, MD3, Valery Hrad, MD4, Paul Cesanek, MD1, Scott Beman, MD1, Hiral Shah, MD5, Shashin Shah, MD6
1Lehigh Valley Health Network, Allentown, PA; 2University of Pittsburgh, Pittsburgh, PA; 3Ascension St. Vincent Anderson, Fishers, IN; 4Monroe Clinic and Hospital/SSM Health, Monroe, WI; 5LVHN/EPGI, Allentown, PA; 6Eastern Pennsylvania Gastroenterology and Liver Specialists, Allentown, PA
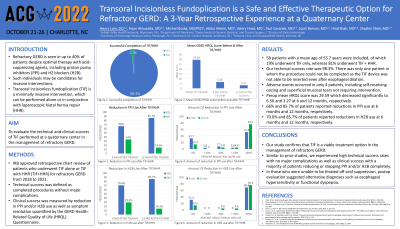
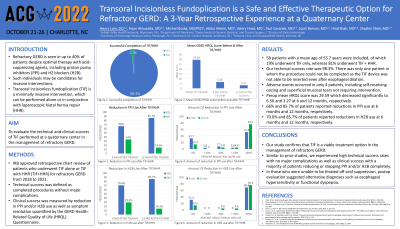
Introduction: Refractory GERD is seen in up to 40% of patients who experience persistent symptoms despite optimal therapy with acid-suppressing agents, including proton pump inhibitors (PPI) and H2 blockers (H2B). Such individuals may be candidates for invasive interventions. Transoral incisionless fundoplication (TIF) is a minimally invasive intervention, which can be performed alone or in conjunction with laparoscopic hiatal hernia repair (HHR). Our study aimed to evaluate the technical and clinical success of TIF performed at a quaternary center in the management of refractory GERD.
Methods: This is an IRB approved retrospective chart review of patients who underwent TIF alone or TIF with HHR (TIF+HHR) for refractory GERD from 2018 to 2021. Technical success was defined as completed procedures without major complications. Clinical success was measured by reduction in PPI and/or H2B use as well as symptom resolution quantified by the GERD HQRL Questionnaire.
Results: A total of 58 patients with a mean age of 55.7 years were included of whom 62.7% were female. 19.0% underwent TIF only, while 81.0% underwent TIF+HHR. Hill grade I, II, III, and IV was respectively present in 9.3%, 32.6%, 44.2%, and 9.3% of patients with a mean hiatal hernia length of 2.36 cm. The technical success rate was 98.3% - there was only one patient in whom the procedure could not be completed as the TIF device was not able to be inserted even after esophageal dilation. At 12 months, 85.7% of patients reported reduction in PPI use of whom 76.2% stopped completely and 9.6% reduced dosing by ≥ 50%. Similar results were seen in those with H2B use with 85.7% of patients stopping completely. Preop mean HQRL score was 29.59 which decreased significantly to 6.56 and 3.27 at 6 and 12 months, respectively. At 12 months, 81.8% reported satisfaction with their condition, whereas 9.1% were neutral and 9.1% were dissatisfied. Complications occurred in 4 patients, including self-resolving oozing and superficial mucosal tears not requiring intervention.
Discussion: Our study confirms that TIF is a viable treatment option in the management of refractory GERD. Similar to prior studies, we experienced high technical success rates with no major complications as well as clinical success with a majority of patients being able to reduce or stop PPI and/or H2B completely. In those who were unable to be titrated off acid suppression, postop evaluation suggested alternative diagnoses such as esophageal hypersensitivity or functional dyspepsia.
Disclosures:
Henry Lam, DO1, Arjan Ahluwalia, MD1, Michal Kloska, MD, PhD2, Abdul Aleem, MD3, Valery Hrad, MD4, Paul Cesanek, MD1, Scott Beman, MD1, Hiral Shah, MD5, Shashin Shah, MD6. D0439 - Transoral Incisionless Fundoplication Is a Safe and Effective Therapeutic Option for Refractory GERD: A 3-Year Retrospective Experience at a Quaternary Center, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Lehigh Valley Health Network, Allentown, PA; 2University of Pittsburgh, Pittsburgh, PA; 3Ascension St. Vincent Anderson, Fishers, IN; 4Monroe Clinic and Hospital/SSM Health, Monroe, WI; 5LVHN/EPGI, Allentown, PA; 6Eastern Pennsylvania Gastroenterology and Liver Specialists, Allentown, PA
Introduction: Refractory GERD is seen in up to 40% of patients who experience persistent symptoms despite optimal therapy with acid-suppressing agents, including proton pump inhibitors (PPI) and H2 blockers (H2B). Such individuals may be candidates for invasive interventions. Transoral incisionless fundoplication (TIF) is a minimally invasive intervention, which can be performed alone or in conjunction with laparoscopic hiatal hernia repair (HHR). Our study aimed to evaluate the technical and clinical success of TIF performed at a quaternary center in the management of refractory GERD.
Methods: This is an IRB approved retrospective chart review of patients who underwent TIF alone or TIF with HHR (TIF+HHR) for refractory GERD from 2018 to 2021. Technical success was defined as completed procedures without major complications. Clinical success was measured by reduction in PPI and/or H2B use as well as symptom resolution quantified by the GERD HQRL Questionnaire.
Results: A total of 58 patients with a mean age of 55.7 years were included of whom 62.7% were female. 19.0% underwent TIF only, while 81.0% underwent TIF+HHR. Hill grade I, II, III, and IV was respectively present in 9.3%, 32.6%, 44.2%, and 9.3% of patients with a mean hiatal hernia length of 2.36 cm. The technical success rate was 98.3% - there was only one patient in whom the procedure could not be completed as the TIF device was not able to be inserted even after esophageal dilation. At 12 months, 85.7% of patients reported reduction in PPI use of whom 76.2% stopped completely and 9.6% reduced dosing by ≥ 50%. Similar results were seen in those with H2B use with 85.7% of patients stopping completely. Preop mean HQRL score was 29.59 which decreased significantly to 6.56 and 3.27 at 6 and 12 months, respectively. At 12 months, 81.8% reported satisfaction with their condition, whereas 9.1% were neutral and 9.1% were dissatisfied. Complications occurred in 4 patients, including self-resolving oozing and superficial mucosal tears not requiring intervention.
Discussion: Our study confirms that TIF is a viable treatment option in the management of refractory GERD. Similar to prior studies, we experienced high technical success rates with no major complications as well as clinical success with a majority of patients being able to reduce or stop PPI and/or H2B completely. In those who were unable to be titrated off acid suppression, postop evaluation suggested alternative diagnoses such as esophageal hypersensitivity or functional dyspepsia.
Disclosures:
Henry Lam indicated no relevant financial relationships.
Arjan Ahluwalia indicated no relevant financial relationships.
Michal Kloska indicated no relevant financial relationships.
Abdul Aleem indicated no relevant financial relationships.
Valery Hrad indicated no relevant financial relationships.
Paul Cesanek: Intuitive Surgical, Inc. – Proctor.
Scott Beman indicated no relevant financial relationships.
Hiral Shah: Abbvie – Speakers Bureau.
Shashin Shah indicated no relevant financial relationships.
Henry Lam, DO1, Arjan Ahluwalia, MD1, Michal Kloska, MD, PhD2, Abdul Aleem, MD3, Valery Hrad, MD4, Paul Cesanek, MD1, Scott Beman, MD1, Hiral Shah, MD5, Shashin Shah, MD6. D0439 - Transoral Incisionless Fundoplication Is a Safe and Effective Therapeutic Option for Refractory GERD: A 3-Year Retrospective Experience at a Quaternary Center, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
