Back

Poster Session D - Tuesday Morning
Category: Liver
D0483 - Association of Effective Patient Communication With Hepatitis B Vaccine Coverage in the United States
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Jasper Seth Yao, MD
Einstein Healthcare Network
Philadelphia, PA
Presenting Author(s)
Jasper Seth Yao, MD1, Edward Christopher Dee, MD2, Joseph Paguio, MD1, Troy Amen, MD3, Sonali Paul, MD, MS4, Adjoa Anyane-Yeboa, MD5
1Einstein Healthcare Network, Philadelphia, PA; 2Memorial Sloan Kettering Cancer Center, New York, NY; 3Hospital for Special Surgery, New York, NY; 4The University of Chicago Medicine, Chicago, IL; 5Massachusetts General Hospital, Boston, MA
Introduction: In 2018, the prevalence of past or present hepatitis B virus (HBV) infection in the United States was 4.3%. Evidence of HBV infection was highest among foreign-born adults. As of 2012, the prevalence of hepatitis B vaccine-induced immunity was 25% in the US. Meanwhile, the CDC recommends HBV vaccination for adults who are at-risk for contracting the infection, including sexually-active adults with more than one partner in the past 6 months and those exposed to blood among others.
Methods: The NHIS was queried for respondents in 2017—the only year in which a set of questions were included to assess patient access to effective communication in the past 12 months. Sample-weight adjusted multivariable logistic regressions defined adjusted odds ratios (AOR) and 95% confidence intervals (CI) of receiving the hepatitis B vaccine with response to one of the five questions on effective patient communication and cultural competency as the independent variable of interest, while controlling for relevant sociodemographic and clinical variables. Statistical analyses were conducted using Stata/IC 16.1 (StataCorp) with α=0.05.
Results: 19,371 participants aged 18 or above responded to the effective patient communication and cultural competency questions, with a median age of 54 (IQR 37-67). 66.79% were non-Hispanic white, 54.51% were female, 6.64% were uninsured, 3.17% were non-English speaking, and 16.04% were foreign-born. Respondents who were asked about their opinions and beliefs regarding their care (aOR 1.28, 95% CI 1.18-1.40, p< 0.001) and those who were given easy-to-understand information (aOR 1.18, 95% CI 1.00-1.40, p=0.04) were significantly more likely to receive HBV vaccination compared to their counterparts. Non-English-speaking participants (aOR=0.64, 95% CI, 0.46-0.89, p=.01), older, and uninsured individuals were less likely to have received any HBV vaccination (p< .001).
Discussion: Being inoculated against hepatitis B was positively correlated with measures of effective patient communication, and negatively correlated with being a non-English speaker, older, and uninsured. These inequities can be partially explained by implicit biases among healthcare providers, poor health literacy, and lack of healthcare access among others. Lack of effective patient communication contributes to those disparities, while effective patient communication improves outcomes in vaccination, healthcare, and satisfaction. Future studies and policies can build upon these comprehensive findings.
Disclosures:
Jasper Seth Yao, MD1, Edward Christopher Dee, MD2, Joseph Paguio, MD1, Troy Amen, MD3, Sonali Paul, MD, MS4, Adjoa Anyane-Yeboa, MD5. D0483 - Association of Effective Patient Communication With Hepatitis B Vaccine Coverage in the United States, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Einstein Healthcare Network, Philadelphia, PA; 2Memorial Sloan Kettering Cancer Center, New York, NY; 3Hospital for Special Surgery, New York, NY; 4The University of Chicago Medicine, Chicago, IL; 5Massachusetts General Hospital, Boston, MA
Introduction: In 2018, the prevalence of past or present hepatitis B virus (HBV) infection in the United States was 4.3%. Evidence of HBV infection was highest among foreign-born adults. As of 2012, the prevalence of hepatitis B vaccine-induced immunity was 25% in the US. Meanwhile, the CDC recommends HBV vaccination for adults who are at-risk for contracting the infection, including sexually-active adults with more than one partner in the past 6 months and those exposed to blood among others.
Methods: The NHIS was queried for respondents in 2017—the only year in which a set of questions were included to assess patient access to effective communication in the past 12 months. Sample-weight adjusted multivariable logistic regressions defined adjusted odds ratios (AOR) and 95% confidence intervals (CI) of receiving the hepatitis B vaccine with response to one of the five questions on effective patient communication and cultural competency as the independent variable of interest, while controlling for relevant sociodemographic and clinical variables. Statistical analyses were conducted using Stata/IC 16.1 (StataCorp) with α=0.05.
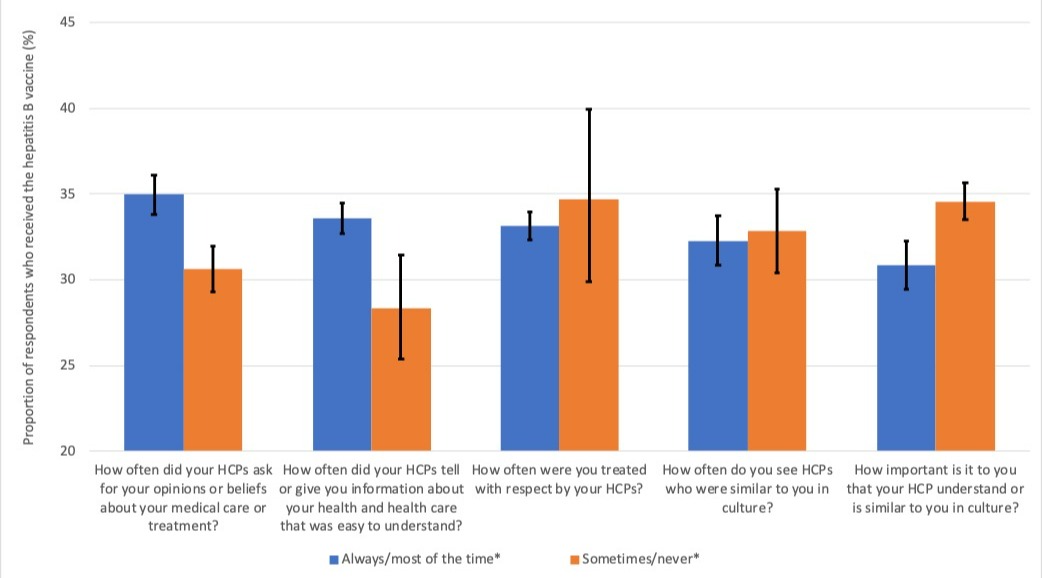
Results: 19,371 participants aged 18 or above responded to the effective patient communication and cultural competency questions, with a median age of 54 (IQR 37-67). 66.79% were non-Hispanic white, 54.51% were female, 6.64% were uninsured, 3.17% were non-English speaking, and 16.04% were foreign-born. Respondents who were asked about their opinions and beliefs regarding their care (aOR 1.28, 95% CI 1.18-1.40, p< 0.001) and those who were given easy-to-understand information (aOR 1.18, 95% CI 1.00-1.40, p=0.04) were significantly more likely to receive HBV vaccination compared to their counterparts. Non-English-speaking participants (aOR=0.64, 95% CI, 0.46-0.89, p=.01), older, and uninsured individuals were less likely to have received any HBV vaccination (p< .001).
Discussion: Being inoculated against hepatitis B was positively correlated with measures of effective patient communication, and negatively correlated with being a non-English speaker, older, and uninsured. These inequities can be partially explained by implicit biases among healthcare providers, poor health literacy, and lack of healthcare access among others. Lack of effective patient communication contributes to those disparities, while effective patient communication improves outcomes in vaccination, healthcare, and satisfaction. Future studies and policies can build upon these comprehensive findings.
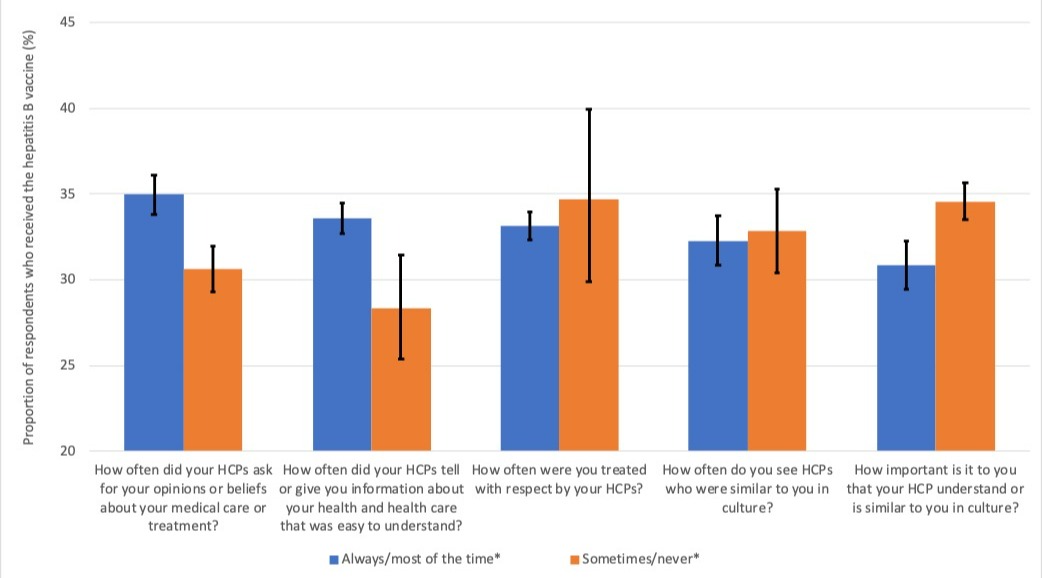
Figure: Weighted proportionsa of respondents aged ≥18 years who received the hepatitis B vaccine stratified by answers to the five cultural competency measures from the NHIS 2017.
HCP = healthcare provider
*asterisk denotes statistical significance at p<0.05
*Very/somewhat important (blue) vs. slightly/not at all important (orange) were respondents’ answers to the 5th survey question
a Adult respondents self-reported their history of receiving “any hepatitis B vaccine”. In addition to answers to one of the five cultural competency survey questions, the models were also adjusted for sociodemographic and clinical variables including age, sex, race (non-Hispanic white, non-Hispanic black, Hispanic, Asian, or other), sexual orientation (heterosexual / ”straight, that is, not lesbian or gay” or lesbian / gay / bisexual / ”something else” / unknown), insurance status (insured or non-insured), nativity (US mainland-born, non-mainland US territory-born, or foreign-born), language spoken (English speaker or non-English speaker), smoking (smoker vs non-smoker), educational attainment (Grade 8, Grade 12 with no diploma, high school diploma, some college, Bachelor’s degree, or advanced degree), usual place of care (with or without), socioeconomic status as the ratio of family income to the poverty threshold (<1.00, 1.00-1.99, 2.00 or greater), presence of comorbidities considered high-risk for worse influenza outcomes according to the Advisory Committee on Immunization Practices (no comorbidity, one comorbidity, or two or more comorbidities).
HCP = healthcare provider
*asterisk denotes statistical significance at p<0.05
*Very/somewhat important (blue) vs. slightly/not at all important (orange) were respondents’ answers to the 5th survey question
a Adult respondents self-reported their history of receiving “any hepatitis B vaccine”. In addition to answers to one of the five cultural competency survey questions, the models were also adjusted for sociodemographic and clinical variables including age, sex, race (non-Hispanic white, non-Hispanic black, Hispanic, Asian, or other), sexual orientation (heterosexual / ”straight, that is, not lesbian or gay” or lesbian / gay / bisexual / ”something else” / unknown), insurance status (insured or non-insured), nativity (US mainland-born, non-mainland US territory-born, or foreign-born), language spoken (English speaker or non-English speaker), smoking (smoker vs non-smoker), educational attainment (Grade 8, Grade 12 with no diploma, high school diploma, some college, Bachelor’s degree, or advanced degree), usual place of care (with or without), socioeconomic status as the ratio of family income to the poverty threshold (<1.00, 1.00-1.99, 2.00 or greater), presence of comorbidities considered high-risk for worse influenza outcomes according to the Advisory Committee on Immunization Practices (no comorbidity, one comorbidity, or two or more comorbidities).
Disclosures:
Jasper Seth Yao indicated no relevant financial relationships.
Edward Christopher Dee indicated no relevant financial relationships.
Joseph Paguio indicated no relevant financial relationships.
Troy Amen indicated no relevant financial relationships.
Sonali Paul indicated no relevant financial relationships.
Adjoa Anyane-Yeboa indicated no relevant financial relationships.
Jasper Seth Yao, MD1, Edward Christopher Dee, MD2, Joseph Paguio, MD1, Troy Amen, MD3, Sonali Paul, MD, MS4, Adjoa Anyane-Yeboa, MD5. D0483 - Association of Effective Patient Communication With Hepatitis B Vaccine Coverage in the United States, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
