Back

Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0028 - Pleomorphic Sarcoma Presenting as Pancreatitis, Panniculitis and Polyarthritis Syndrome
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- AS
Ann Saliares, BS, DO
St. Joseph Mercy Hospital Ann Arbor
Ypsilanti, MI
Presenting Author(s)
Ann Saliares, BS, DO1, Elliot Berinstein, BSc, MSc, MD1, Wael Al-Yaman, MD2, Naresh Gunaratnam, MD, FACG3
1St. Joseph Mercy Hospital Ann Arbor, Ypsilanti, MI; 2St. Joseph Mercy Hospital, Ypsilanti, MI; 3Huron Gastro, Ypsilanti, MI
Introduction: Pancreatitis, Panniculitis and Polyarthritis Syndrome (PPP) is a rare triad that develops with chronic or acute pancreatitis and pancreatic cancer. Roughly 50% of PPP patients deny abdominal pain, delaying identification of a pancreatic etiology. Treatment includes symptomatic control and resolving the pancreatic disease. In a review of 59 PPP cases, 11.9% were attributed to pancreatic cancer. None were due to pancreatic sarcomas which account for 1% of pancreatic cancer. To our knowledge, we report the first case of pleomorphic sarcoma presenting as PPP.
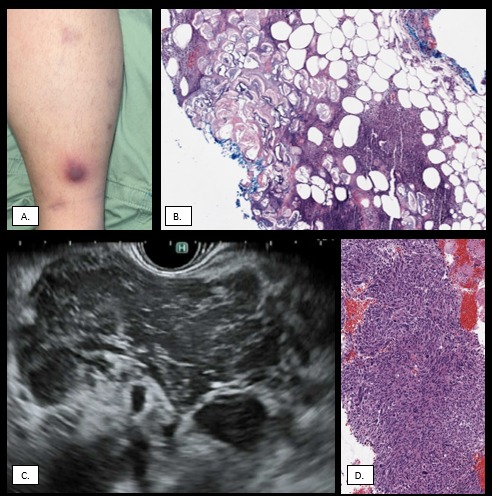
Case Description/Methods: An 18-year-old male with no medical history presented for fever and progressive joint pain. He denied respiratory symptoms, abdominal pain, dysuria, or rash. Physical exam revealed erythematous, tender nodules on his shins with ankle, foot and hand swelling. Labs were notable for elevated AST 47, ALT 83, ALP 136 and lipase 9754. Rheumatologic and infectious evaluation was unremarkable. CT imaging revealed a 5.9 x 5 cm solid pancreatic mass with intracystic component. EUS and FNA was completed with histology notable for marked cellular atypia, patchy positivity for CD34, and negative cytokeratin, c-kit, SMA and desmin. While staining was positive for S100, the retained expression of H3K27me was consistent with pleomorphic sarcoma. Skin biopsy showed panniculitis. Patient underwent chemotherapy with plans for surgical resection.
Discussion: PPP is an extra-pancreatic manifestation of pancreatic cancer. While the pathogenesis is unknown, it is thought to be due to circulating pancreatic enzymes causing lipolysis and can present weeks before abdominal pain. Elevated lipase in the serum or synovial fluid increases suspicion for PPP. Despite pancreatic cancer rarely causing PPP, it should not be discounted in patients without abdominal pain or risk factors for pancreatic cancer.
Pleomorphic sarcoma was previously referred to as malignant fibrous histiocytoma due to the spindle cells and significant pleomorphism. Pleomorphic sarcoma is a diagnosis of exclusion and requires careful evaluation to detect cell differentiation. The lack of identifying characteristics on imaging poses a diagnostic challenge. In patients with PPP, symptomatic control is with NSAIDs and steroids; however, resolution depends on definitive treatment of the underlying pancreatic disease. The mainstay of pleomorphic sarcoma remains surgery although chemotherapy and radiation can be used as adjuncts.
Disclosures:
Ann Saliares, BS, DO1, Elliot Berinstein, BSc, MSc, MD1, Wael Al-Yaman, MD2, Naresh Gunaratnam, MD, FACG3. C0028 - Pleomorphic Sarcoma Presenting as Pancreatitis, Panniculitis and Polyarthritis Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1St. Joseph Mercy Hospital Ann Arbor, Ypsilanti, MI; 2St. Joseph Mercy Hospital, Ypsilanti, MI; 3Huron Gastro, Ypsilanti, MI
Introduction: Pancreatitis, Panniculitis and Polyarthritis Syndrome (PPP) is a rare triad that develops with chronic or acute pancreatitis and pancreatic cancer. Roughly 50% of PPP patients deny abdominal pain, delaying identification of a pancreatic etiology. Treatment includes symptomatic control and resolving the pancreatic disease. In a review of 59 PPP cases, 11.9% were attributed to pancreatic cancer. None were due to pancreatic sarcomas which account for 1% of pancreatic cancer. To our knowledge, we report the first case of pleomorphic sarcoma presenting as PPP.
Case Description/Methods: An 18-year-old male with no medical history presented for fever and progressive joint pain. He denied respiratory symptoms, abdominal pain, dysuria, or rash. Physical exam revealed erythematous, tender nodules on his shins with ankle, foot and hand swelling. Labs were notable for elevated AST 47, ALT 83, ALP 136 and lipase 9754. Rheumatologic and infectious evaluation was unremarkable. CT imaging revealed a 5.9 x 5 cm solid pancreatic mass with intracystic component. EUS and FNA was completed with histology notable for marked cellular atypia, patchy positivity for CD34, and negative cytokeratin, c-kit, SMA and desmin. While staining was positive for S100, the retained expression of H3K27me was consistent with pleomorphic sarcoma. Skin biopsy showed panniculitis. Patient underwent chemotherapy with plans for surgical resection.
Discussion: PPP is an extra-pancreatic manifestation of pancreatic cancer. While the pathogenesis is unknown, it is thought to be due to circulating pancreatic enzymes causing lipolysis and can present weeks before abdominal pain. Elevated lipase in the serum or synovial fluid increases suspicion for PPP. Despite pancreatic cancer rarely causing PPP, it should not be discounted in patients without abdominal pain or risk factors for pancreatic cancer.
Pleomorphic sarcoma was previously referred to as malignant fibrous histiocytoma due to the spindle cells and significant pleomorphism. Pleomorphic sarcoma is a diagnosis of exclusion and requires careful evaluation to detect cell differentiation. The lack of identifying characteristics on imaging poses a diagnostic challenge. In patients with PPP, symptomatic control is with NSAIDs and steroids; however, resolution depends on definitive treatment of the underlying pancreatic disease. The mainstay of pleomorphic sarcoma remains surgery although chemotherapy and radiation can be used as adjuncts.
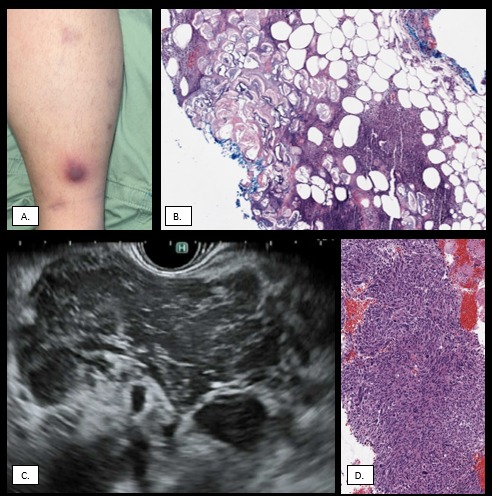
Figure: Figure 1. A) Erythematous, tender nodules on lower extremity at time of presentation. B) Skin biopsy of the left shin. H&E Stain. High power view of the subcutaneous tissue demonstrates fat necrosis with necrotic adipocyte ghosts and basophilic material, consistent with pancreatic panniculitis. C) Endoscopic ultrasound identification of pancreatic head mass measuring 50mm x 60mm. D) Pancreatic mass aspirate. Cell block, H&E Stain. The pancreatic mass aspirate demonstrates a highly cellular pleomorphic sarcoma with frequent bizarre mitotic figures and anaplastic cytology, consistent with an undifferentiated pleomorphic sarcoma.
Disclosures:
Ann Saliares indicated no relevant financial relationships.
Elliot Berinstein indicated no relevant financial relationships.
Wael Al-Yaman indicated no relevant financial relationships.
Naresh Gunaratnam: Lean Medical LLC – Founder & CMO. Satya Health – Founder & CMO.
Ann Saliares, BS, DO1, Elliot Berinstein, BSc, MSc, MD1, Wael Al-Yaman, MD2, Naresh Gunaratnam, MD, FACG3. C0028 - Pleomorphic Sarcoma Presenting as Pancreatitis, Panniculitis and Polyarthritis Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
