Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0065 - The Gallbladder Houdini: A Rare Presentation of Eosinophilic Cholecystitis and Gastroenteritis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Hima Veeramachaneni, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Irtiqa Fazili, MD, Hima Veeramachaneni, MD, Sonali Sakaria, MD
Emory University School of Medicine, Atlanta, GA
Introduction: Eosinophilic gastroenteritis (EG) is an inflammatory condition with eosinophilic infiltration of the GI tract, but biliary tract involvement is rare. We report a rare case of EG with concurrent eosinophilic cholecystitis.
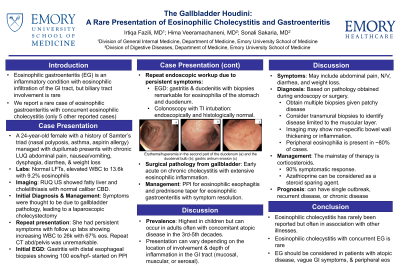
Case Description/Methods: A 24 y/o WF with a history of Samter’s triad (nasal polyposis, asthma, aspirin allergy) managed with dupilumab, presented to the ER with chronic LUQ abdominal pain, N/V, dysphagia, diarrhea, and weight loss. Lab revealed normal LFTs and an elevated WBC to 13.6k with 9.2% eosinophils (eos). RUQ US showed fatty liver and cholelithiasis with normal caliber CBD. She underwent laparoscopic cholecystectomy with surgical pathology revealing early acute on chronic cholecystitis and cholelithiasis with extensive eosinophilic inflammation.
She noted persistent symptoms with follow up labs showing increasing WBC to 26k with 67% eos. Repeat CT scan was unremarkable. Initial EGD showed gastritis with distal esophageal biopsies showing 100 eos/hpf. She was started on PPI. Repeat EGD showed gastritis and duodenitis with biopsies remarkable for eosinophilia of the stomach and proximal small bowel. Colonoscopy with TI intubation was endoscopically normal with normal biopsies of the TI and colon. She was started on PPI for eosinophilic esophagitis and a prednisone taper for eosinophilic gastroenteritis with symptom resolution.
Discussion: The prevalence of EG is highest in children but can occur in adults often with concomitant atopic disease in the 3rd-5th decades. The clinical presentation varies, depending on the depth of inflammation (mucosal, muscular, or serosa) and location of involvement and may include abdominal pain, N/V, diarrhea, and weight loss. Diagnosis is based on pathology obtained during endoscopy or surgery. It is prudent to obtain multiple biopsies given patchy disease and consider transmural biopsies to identify processes limited to the muscular layer. Imaging can show non-specific inflammation. Peripheral eosinophilia is present in ~80% of cases. The mainstay of therapy is corticosteroids, with a 90% symptomatic response. Azathioprine can be considered as a steroid sparing agent.
Eosinophilic cholecystitis has rarely been reported in the literature but often in association with other illnesses. We present a unique case of eosinophilic cholecystitis in a patient with concurrent eosinophilic gastroenteritis. Upon review of the literature only 5 other similar cases have been described.
Disclosures:
Irtiqa Fazili, MD, Hima Veeramachaneni, MD, Sonali Sakaria, MD. D0065 - The Gallbladder Houdini: A Rare Presentation of Eosinophilic Cholecystitis and Gastroenteritis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Emory University School of Medicine, Atlanta, GA
Introduction: Eosinophilic gastroenteritis (EG) is an inflammatory condition with eosinophilic infiltration of the GI tract, but biliary tract involvement is rare. We report a rare case of EG with concurrent eosinophilic cholecystitis.
Case Description/Methods: A 24 y/o WF with a history of Samter’s triad (nasal polyposis, asthma, aspirin allergy) managed with dupilumab, presented to the ER with chronic LUQ abdominal pain, N/V, dysphagia, diarrhea, and weight loss. Lab revealed normal LFTs and an elevated WBC to 13.6k with 9.2% eosinophils (eos). RUQ US showed fatty liver and cholelithiasis with normal caliber CBD. She underwent laparoscopic cholecystectomy with surgical pathology revealing early acute on chronic cholecystitis and cholelithiasis with extensive eosinophilic inflammation.
She noted persistent symptoms with follow up labs showing increasing WBC to 26k with 67% eos. Repeat CT scan was unremarkable. Initial EGD showed gastritis with distal esophageal biopsies showing 100 eos/hpf. She was started on PPI. Repeat EGD showed gastritis and duodenitis with biopsies remarkable for eosinophilia of the stomach and proximal small bowel. Colonoscopy with TI intubation was endoscopically normal with normal biopsies of the TI and colon. She was started on PPI for eosinophilic esophagitis and a prednisone taper for eosinophilic gastroenteritis with symptom resolution.
Discussion: The prevalence of EG is highest in children but can occur in adults often with concomitant atopic disease in the 3rd-5th decades. The clinical presentation varies, depending on the depth of inflammation (mucosal, muscular, or serosa) and location of involvement and may include abdominal pain, N/V, diarrhea, and weight loss. Diagnosis is based on pathology obtained during endoscopy or surgery. It is prudent to obtain multiple biopsies given patchy disease and consider transmural biopsies to identify processes limited to the muscular layer. Imaging can show non-specific inflammation. Peripheral eosinophilia is present in ~80% of cases. The mainstay of therapy is corticosteroids, with a 90% symptomatic response. Azathioprine can be considered as a steroid sparing agent.
Eosinophilic cholecystitis has rarely been reported in the literature but often in association with other illnesses. We present a unique case of eosinophilic cholecystitis in a patient with concurrent eosinophilic gastroenteritis. Upon review of the literature only 5 other similar cases have been described.
Disclosures:
Irtiqa Fazili indicated no relevant financial relationships.
Hima Veeramachaneni indicated no relevant financial relationships.
Sonali Sakaria indicated no relevant financial relationships.
Irtiqa Fazili, MD, Hima Veeramachaneni, MD, Sonali Sakaria, MD. D0065 - The Gallbladder Houdini: A Rare Presentation of Eosinophilic Cholecystitis and Gastroenteritis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
