Back

Poster Session B - Monday Morning
Category: IBD
B0437 - Incidental Finding of Intestinal Spirochetosis in a Patient With Inflammatory Bowel Disease
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- ZA
Zarir M. Ahmed, DO
St. Louis University Hospital
Ballwin, MO
Presenting Author(s)
Zarir M. Ahmed, DO1, Mashkurul Haque, 2, Michelle Baliss, DO2, Laith Numan, MD2, Soumojit Ghosh, MD2, Thomas Fay, MD3, Danielle Carpenter, MD4, Christine Boumitri, MD4
1St. Louis University Hospital, Ballwin, MO; 2Saint Louis University, St. Louis, MO; 3Saint Louis University School of Medicine, St. Louis, MO; 4St. Louis University, St. Louis, MO
Introduction: Intestinal spirochetosis (IS) is an infection most commonly caused by Brachyspira aalborgi, a gram-negative spirochete. Early on, IS was thought to be most commonly associated with HIV infection, but recent studies have shown a link to patients with a wide variety of risk factors, including IBD. We present a case of an IBD patient with incidental ly intestinal spirochetosis identified on colonic biopsy.
Case Description/Methods: A 40-year-old female with a history of stricturing ileocolonic Crohn's disease was seen in gastroenterology clinic for follow-up. She was diagnosed with Crohn's disease in 2019, initially treated with adalimumab; however, due to antibody formation, she was transitioned to ustekinumab. She reported 1 to 2 formed bowel movements daily and no other significant symptoms such as abdominal pain, nausea, rashes, sores, or weight loss. She underwent colonoscopy for disease monitoring, which revealed normal colon, ileal stricture and 1 small ileal erosion but otherwise no signs of active disease. Incidentally, her pathology revealed intestinal spirochetes. Of note, the patient used to work as a veterinarian and has a dog at home.
Discussion: IS is typically asymptomatic but may present with chronic, watery diarrhea or vague abdominal pain. Diagnosis is made incidentally on histology of colonic mucosal biopsies. Some reports have described polypoid and erythematous lesions associated with IS, but they are typically not easily identifiable.
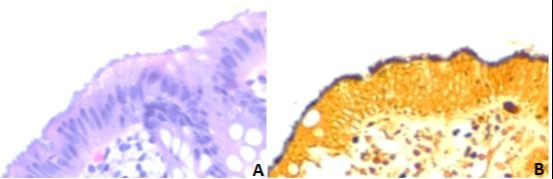
Histologically, silver stains or immunostains for Treponema pallidum may be necessary to identify these organisms . A hallmark of IS is the “false brush border” formed by a band of spirochetes adhering to the epithelial layer .
Originally, IS was mainly found in areas of low socioeconomic status in veterinary medicine. Human colonization has been observed more recently predominantly in HIV and homosexual male populations. IBD patients are at a higher risk of infection due to immunocompromised status.
Asymptomatic patients do not require treatment. However, for those requiring treatment, a trial of metronidazole can be use. One case report documented IS in an IBD patient with symptoms of abdominal pain and watery diarrhea that was successfully treated with metronidazole leading to complete resolution of symptoms .
This case highlights a rare etiology of chronic diarrhea that should be considered, especially in immunocompromised patients with no other clear cause of symptoms.
Disclosures:
Zarir M. Ahmed, DO1, Mashkurul Haque, 2, Michelle Baliss, DO2, Laith Numan, MD2, Soumojit Ghosh, MD2, Thomas Fay, MD3, Danielle Carpenter, MD4, Christine Boumitri, MD4. B0437 - Incidental Finding of Intestinal Spirochetosis in a Patient With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1St. Louis University Hospital, Ballwin, MO; 2Saint Louis University, St. Louis, MO; 3Saint Louis University School of Medicine, St. Louis, MO; 4St. Louis University, St. Louis, MO
Introduction: Intestinal spirochetosis (IS) is an infection most commonly caused by Brachyspira aalborgi, a gram-negative spirochete. Early on, IS was thought to be most commonly associated with HIV infection, but recent studies have shown a link to patients with a wide variety of risk factors, including IBD. We present a case of an IBD patient with incidental ly intestinal spirochetosis identified on colonic biopsy.
Case Description/Methods: A 40-year-old female with a history of stricturing ileocolonic Crohn's disease was seen in gastroenterology clinic for follow-up. She was diagnosed with Crohn's disease in 2019, initially treated with adalimumab; however, due to antibody formation, she was transitioned to ustekinumab. She reported 1 to 2 formed bowel movements daily and no other significant symptoms such as abdominal pain, nausea, rashes, sores, or weight loss. She underwent colonoscopy for disease monitoring, which revealed normal colon, ileal stricture and 1 small ileal erosion but otherwise no signs of active disease. Incidentally, her pathology revealed intestinal spirochetes. Of note, the patient used to work as a veterinarian and has a dog at home.
Discussion: IS is typically asymptomatic but may present with chronic, watery diarrhea or vague abdominal pain. Diagnosis is made incidentally on histology of colonic mucosal biopsies. Some reports have described polypoid and erythematous lesions associated with IS, but they are typically not easily identifiable.
Histologically, silver stains or immunostains for Treponema pallidum may be necessary to identify these organisms . A hallmark of IS is the “false brush border” formed by a band of spirochetes adhering to the epithelial layer .
Originally, IS was mainly found in areas of low socioeconomic status in veterinary medicine. Human colonization has been observed more recently predominantly in HIV and homosexual male populations. IBD patients are at a higher risk of infection due to immunocompromised status.
Asymptomatic patients do not require treatment. However, for those requiring treatment, a trial of metronidazole can be use. One case report documented IS in an IBD patient with symptoms of abdominal pain and watery diarrhea that was successfully treated with metronidazole leading to complete resolution of symptoms .
This case highlights a rare etiology of chronic diarrhea that should be considered, especially in immunocompromised patients with no other clear cause of symptoms.
Figure: A – Attached to the luminal border are fuzzy basophilic structures, recall that colonic mucosa does not have a microvillus border, and even if it did, this is too thick (hematoxylin and eosin 40X). B – The organisms are positive on silver based stains
Disclosures:
Zarir Ahmed indicated no relevant financial relationships.
Mashkurul Haque indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Laith Numan indicated no relevant financial relationships.
Soumojit Ghosh indicated no relevant financial relationships.
Thomas Fay indicated no relevant financial relationships.
Danielle Carpenter indicated no relevant financial relationships.
Christine Boumitri indicated no relevant financial relationships.
Zarir M. Ahmed, DO1, Mashkurul Haque, 2, Michelle Baliss, DO2, Laith Numan, MD2, Soumojit Ghosh, MD2, Thomas Fay, MD3, Danielle Carpenter, MD4, Christine Boumitri, MD4. B0437 - Incidental Finding of Intestinal Spirochetosis in a Patient With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
