Back

Poster Session D - Tuesday Morning
Category: Liver
D0503 - A Case Series of Combined Portal Vein Recanalization and Transjugular Intrahepatic Portosystemic Shunt Placement in Cirrhotic Patients
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Nicholas Forrister, MD
University of Alabama at Birmingham
Birmingham, Alabama
Presenting Author(s)
Nicholas Forrister, MD1, Mahmoud Aryan, MD1, Mohamed Shoreibah, MD2
1University of Alabama at Birmingham, Birmingham, AL; 2University of Alabama Birmingham, Birmingham, AL
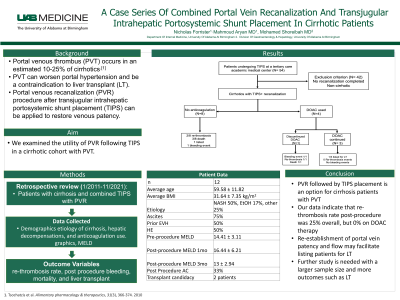
Introduction: Portal venous thrombus (PVT) occurs in an estimated 10-25% of cirrhotics (1). PVT can worsen portal hypertension and be a contraindication to liver transplant (LT). Portal venous recanalization (PVR) procedure after transjugular intrahepatic portosystemic shunt placement (TIPS) can be applied to restore venous patency. We examined the utility of PVR following TIPS in a cirrhotic cohort with PVT.
Methods: We performed a retrospective review of patients who had TIPS placement and PVT between 2011-2021 at a tertiary medical center. Inclusion criteria consisted of combined PVR with TIPS in cirrhotic patients. Demographic data were collected alongside data on etiology of cirrhosis, hepatic decompensations, and anticoagulation use. Model for end stage liver disease (MELD) score was calculated pre and post procedure. Outcome variables included re-thrombosis, post procedure bleeding, mortality, and LT. Descriptive statistics were represented by mean ± SD for continuous variables and frequency percentage for categorical variables.
Results: 12 patients were found with cirrhosis that had combined TIPS with PVR. Average age and BMI at procedure were 59.58 ± 11.82 years and 31.64 ± 7.35 kg/m2. Cirrhosis etiologies included NASH (50%), ETOH (17%), combined NASH/ETOH (8%), or other (25%). Baseline hepatic decompensations included ascites (75%), prior variceal bleed (50%), and hepatic encephalopathy (50%). Four (33%) patients were placed on anticoagulation (AC) post procedure. Overall re-thrombosis rate was 3/12 (25%). Amongst these 3 patients, 1 suffered re-thrombosis after AC had been suspended following variceal bleed. No other post-procedure bleeding or re-thrombosis were reported in the remaining AC cohort. Average pre-procedure MELD score was 14.41 ± 3.11, which increased to 16.44 ± 6.21 at one month, but decreased to 13 ± 2.94 at 6 months. Two patients were listed for LT, with the remaining 10 patients being deemed not candidates. Overall mortality rate was 33%, and no patients received LT.
Discussion: PVR followed by TIPS placement is an option for cirrhotics with PVT. Our data indicate that re-thrombosis rate post-procedure was 25% overall, but 0% on DOAC therapy. Re-establishment of portal vein patency and flow may facilitate listing patients for LT as shown in our case series. Further studies with a larger patient population are needed to report on outcomes including LT.
1. Tsochatzis et al. Alimentary pharmacology & therapeutics 31 (3), 366-374. 2010

Disclosures:
Nicholas Forrister, MD1, Mahmoud Aryan, MD1, Mohamed Shoreibah, MD2. D0503 - A Case Series of Combined Portal Vein Recanalization and Transjugular Intrahepatic Portosystemic Shunt Placement in Cirrhotic Patients, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2University of Alabama Birmingham, Birmingham, AL
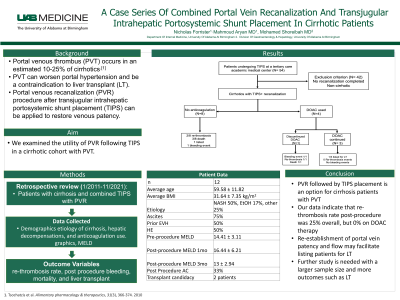
Introduction: Portal venous thrombus (PVT) occurs in an estimated 10-25% of cirrhotics (1). PVT can worsen portal hypertension and be a contraindication to liver transplant (LT). Portal venous recanalization (PVR) procedure after transjugular intrahepatic portosystemic shunt placement (TIPS) can be applied to restore venous patency. We examined the utility of PVR following TIPS in a cirrhotic cohort with PVT.
Methods: We performed a retrospective review of patients who had TIPS placement and PVT between 2011-2021 at a tertiary medical center. Inclusion criteria consisted of combined PVR with TIPS in cirrhotic patients. Demographic data were collected alongside data on etiology of cirrhosis, hepatic decompensations, and anticoagulation use. Model for end stage liver disease (MELD) score was calculated pre and post procedure. Outcome variables included re-thrombosis, post procedure bleeding, mortality, and LT. Descriptive statistics were represented by mean ± SD for continuous variables and frequency percentage for categorical variables.
Results: 12 patients were found with cirrhosis that had combined TIPS with PVR. Average age and BMI at procedure were 59.58 ± 11.82 years and 31.64 ± 7.35 kg/m2. Cirrhosis etiologies included NASH (50%), ETOH (17%), combined NASH/ETOH (8%), or other (25%). Baseline hepatic decompensations included ascites (75%), prior variceal bleed (50%), and hepatic encephalopathy (50%). Four (33%) patients were placed on anticoagulation (AC) post procedure. Overall re-thrombosis rate was 3/12 (25%). Amongst these 3 patients, 1 suffered re-thrombosis after AC had been suspended following variceal bleed. No other post-procedure bleeding or re-thrombosis were reported in the remaining AC cohort. Average pre-procedure MELD score was 14.41 ± 3.11, which increased to 16.44 ± 6.21 at one month, but decreased to 13 ± 2.94 at 6 months. Two patients were listed for LT, with the remaining 10 patients being deemed not candidates. Overall mortality rate was 33%, and no patients received LT.
Discussion: PVR followed by TIPS placement is an option for cirrhotics with PVT. Our data indicate that re-thrombosis rate post-procedure was 25% overall, but 0% on DOAC therapy. Re-establishment of portal vein patency and flow may facilitate listing patients for LT as shown in our case series. Further studies with a larger patient population are needed to report on outcomes including LT.
1. Tsochatzis et al. Alimentary pharmacology & therapeutics 31 (3), 366-374. 2010

Figure: Figure 1. A cohort of patients with portal venous thrombosis (PVT) who had transjugular intrahepatic portosystemic shunt placement (TIPS) at a tertiary medical center were retrospectively selected for analysis. Only patients with cirrhosis who had TIPS and portal venous recanalizatoin were included in our study. Data were collected regarding use of direct oral anticoagulants (DOACs), post procedure re-thrombosis, bleeding events, liver transplant (LT) and death.
Disclosures:
Nicholas Forrister indicated no relevant financial relationships.
Mahmoud Aryan indicated no relevant financial relationships.
Mohamed Shoreibah indicated no relevant financial relationships.
Nicholas Forrister, MD1, Mahmoud Aryan, MD1, Mohamed Shoreibah, MD2. D0503 - A Case Series of Combined Portal Vein Recanalization and Transjugular Intrahepatic Portosystemic Shunt Placement in Cirrhotic Patients, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
