Back


Poster Session C - Monday Afternoon
Category: Interventional Endoscopy
C0469 - ERCP via Gastrostomy: A Work Around for Esophageal Stricture or Obstruction
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Savan Kothadia, MD
Warren Alpert Medical School of Brown University
Providence, RI
Presenting Author(s)
Savan Kothadia, MD1, May Min, MD2, Fadlallah Habr, MD3, Sarah M. Hyder, MD, MBA4
1Warren Alpert Medical School of Brown University , Providence, RI; 2Brown University, Providence, RI; 3Warren Alpert Medical School of Brown University, East Providence, RI; 4Lifespan Physician Group - Brown University, East Providence, RI
Introduction: In the setting of biliary obstruction, endoscopic retrograde cholangiopancreatography (ERCP) can be a life-saving intervention. Most often performed via the trans-oral approach, there are indications of ERCP via gastrostomy (GERCP), largely for patients with altered anatomy from Roux-en-Y gastric bypass surgery. Few reports exist regarding GERCP in the setting of esophageal obstruction or stricture. We present a patient with complete esophageal obstruction with subsequent percutaneous gastrostomy (PEG) tube requiring GERCP with a pediatric duodenoscope for acute management of choledocholithiasis.
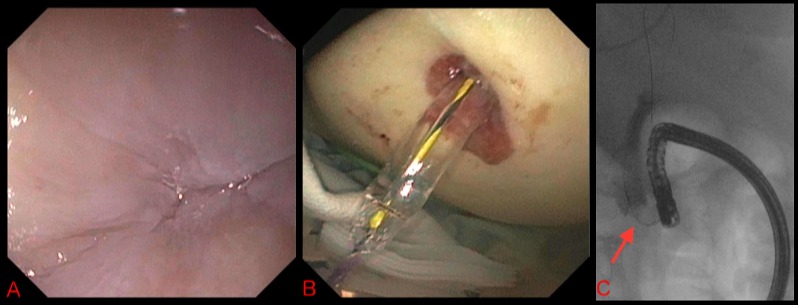
Case Description/Methods: An 84-year-old female with history of a severe benign esophageal stricture refractory to serial dilations, esophageal stenting, and ultimately requiring 20 Fr PEG placement presented with back pain after a mechanical fall. Computed-tomography abdomen/pelvis: intra- and extra-hepatic biliary ductal dilatation with an 8 mm density in the distal common bile duct and a distended gallbladder. Labs: AST/ALT 68/89 IU/L, alkaline phosphatase 610 IU/L, and total bilirubin 2.7 mg. Magnetic resonance cholangiopancreatography confirmed choledocholithiasis. Endoscopic management was the only viable option due to poor surgical candidacy. ERCP via a trans-oral approach was attempted, but the esophageal stricture was completely stenosed, precluding passage of a 0.035 inch guidewire (Image A). The external PEG tube was removed and the gastrostomy stoma was dilated using a 12mm biliary balloon dilator under fluoroscopic guidance (Image B). An Olympus PJF-160 7.5mm diameter duodenoscope was passed through the stoma into the duodenum and the bile duct was cannulated. Fluoroscopy revealed 15mm duct dilation with a 10mm distal filling defect. Stone removal was accomplished via sphincterotomy and balloon, dilation-assisted-stone extraction (Image C). A 20 Fr externally replaceable PEG tube was placed at the stoma site at the end of the procedure.
Discussion: This case demonstrates an alternative approach to an arduous ERCP in a patient with a severe esophageal stricture which was not amenable to dilation or esophageal stenting. GERCP requires extra vigilance due to technical challenges related to positioning and thermal injury risk with a small caliber scope tip, but can serve as another option in an interventional endoscopist’s arsenal for managing biliary disease in patients with esophageal strictures.
Disclosures:
Savan Kothadia, MD1, May Min, MD2, Fadlallah Habr, MD3, Sarah M. Hyder, MD, MBA4. C0469 - ERCP via Gastrostomy: A Work Around for Esophageal Stricture or Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Warren Alpert Medical School of Brown University , Providence, RI; 2Brown University, Providence, RI; 3Warren Alpert Medical School of Brown University, East Providence, RI; 4Lifespan Physician Group - Brown University, East Providence, RI
Introduction: In the setting of biliary obstruction, endoscopic retrograde cholangiopancreatography (ERCP) can be a life-saving intervention. Most often performed via the trans-oral approach, there are indications of ERCP via gastrostomy (GERCP), largely for patients with altered anatomy from Roux-en-Y gastric bypass surgery. Few reports exist regarding GERCP in the setting of esophageal obstruction or stricture. We present a patient with complete esophageal obstruction with subsequent percutaneous gastrostomy (PEG) tube requiring GERCP with a pediatric duodenoscope for acute management of choledocholithiasis.
Case Description/Methods: An 84-year-old female with history of a severe benign esophageal stricture refractory to serial dilations, esophageal stenting, and ultimately requiring 20 Fr PEG placement presented with back pain after a mechanical fall. Computed-tomography abdomen/pelvis: intra- and extra-hepatic biliary ductal dilatation with an 8 mm density in the distal common bile duct and a distended gallbladder. Labs: AST/ALT 68/89 IU/L, alkaline phosphatase 610 IU/L, and total bilirubin 2.7 mg. Magnetic resonance cholangiopancreatography confirmed choledocholithiasis. Endoscopic management was the only viable option due to poor surgical candidacy. ERCP via a trans-oral approach was attempted, but the esophageal stricture was completely stenosed, precluding passage of a 0.035 inch guidewire (Image A). The external PEG tube was removed and the gastrostomy stoma was dilated using a 12mm biliary balloon dilator under fluoroscopic guidance (Image B). An Olympus PJF-160 7.5mm diameter duodenoscope was passed through the stoma into the duodenum and the bile duct was cannulated. Fluoroscopy revealed 15mm duct dilation with a 10mm distal filling defect. Stone removal was accomplished via sphincterotomy and balloon, dilation-assisted-stone extraction (Image C). A 20 Fr externally replaceable PEG tube was placed at the stoma site at the end of the procedure.
Discussion: This case demonstrates an alternative approach to an arduous ERCP in a patient with a severe esophageal stricture which was not amenable to dilation or esophageal stenting. GERCP requires extra vigilance due to technical challenges related to positioning and thermal injury risk with a small caliber scope tip, but can serve as another option in an interventional endoscopist’s arsenal for managing biliary disease in patients with esophageal strictures.
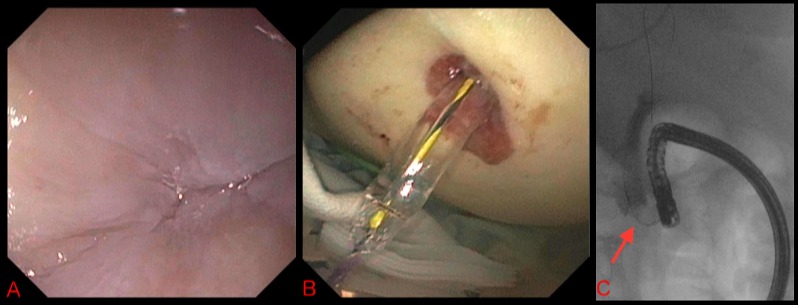
Figure: A) Upper endoscopy showing complete esophageal stenosis B) Dilation of gastrostomy stoma with 12mm biliary balloon dilator C) Cholangiogram showing 12mm balloon dilator in the common bile duct with filling defect consistent with stone
Disclosures:
Savan Kothadia indicated no relevant financial relationships.
May Min indicated no relevant financial relationships.
Fadlallah Habr indicated no relevant financial relationships.
Sarah Hyder indicated no relevant financial relationships.
Savan Kothadia, MD1, May Min, MD2, Fadlallah Habr, MD3, Sarah M. Hyder, MD, MBA4. C0469 - ERCP via Gastrostomy: A Work Around for Esophageal Stricture or Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
