Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0038 - A Case of Bilioptysis After Transarterial Radioembolization of Primary Cholangiocarcinoma
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- WG
William C. Green, MD
Wake Forest University School of Medicine
Winston-Salem, NC
Presenting Author(s)
William C. Green, MD, Meehir Shah, MD, William Lippert, MD
Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Bilioptysis is a rare clinical finding that can be alarming to patients. It is commonly associated with hydatid cysts, trauma, or malignancy. Bilioptysis is typically caused by a bronchobiliary fistula (BBF), but can be secondary to any manipulation of the normal liver architecture adjacent to the diaphragm. We present a rare case of bilioptysis caused by a BBF secondary to transarterial radioembolization (TARE).
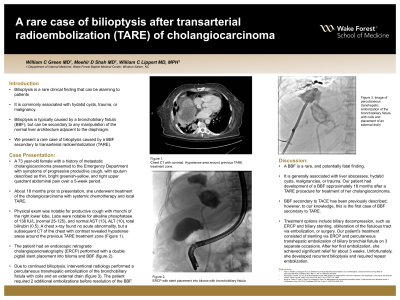
Case Description/Methods: A 73 year-old female with a history of metastatic cholangiocarcinoma presented to the ED with symptoms of progressive productive cough, with sputum described as thin, bright greenish-yellow, and right upper quadrant abdominal pain over a 5-week period. About 18 months prior to presentation, she underwent treatment of the cholangiocarcinoma with systemic chemotherapy and local TARE. Physical exam was notable for productive cough with rhonchi of the right lower lobe. Labs were notable for alkaline phosphatase of 138 IU/L (normal 25-125), and normal AST (13), ALT (10), total bilirubin (0.5). A chest x-ray found no acute abnormality, but a subsequent CT of the chest with contrast revealed hypodense areas around the previous TARE treatment zone. The patient had an endoscopic retrograde cholangiopancreatography performed with a double pigtail stent placement into biloma and BBF. Due to continued bilioptysis, interventional radiology performed a percutaneous transhepatic embolization of the bronchobiliary fistula with coils and an external drain. The patient required 2 additional embolizations before resolution of the BBF.
Discussion: A BBF is a rare, and potentially fatal finding. It is generally associated with liver abscesses, hydatid cysts, malignancies, or trauma. Our patient had development of a BBF approximately 18 months after a TARE procedure for treatment of her cholangiocarcinoma. BBF secondary to TACE has been previously described; however, to our knowledge, this is the first case of BBF secondary to TARE. Treatment options include biliary decompression, such as ERCP and biliary stenting, obliteration of the fistulous tract via embolization, or surgery. Our patient's treatment consisted of stenting via ERCP and percutaneous transhepatic embolization of biliary bronchial fistula on 3 separate occasions. After her first embolization, she achieved significant relief for about 3 weeks. Unfortunately, she developed recurrent bilioptysis and required repeat embolization.

Disclosures:
William C. Green, MD, Meehir Shah, MD, William Lippert, MD. B0038 - A Case of Bilioptysis After Transarterial Radioembolization of Primary Cholangiocarcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Bilioptysis is a rare clinical finding that can be alarming to patients. It is commonly associated with hydatid cysts, trauma, or malignancy. Bilioptysis is typically caused by a bronchobiliary fistula (BBF), but can be secondary to any manipulation of the normal liver architecture adjacent to the diaphragm. We present a rare case of bilioptysis caused by a BBF secondary to transarterial radioembolization (TARE).
Case Description/Methods: A 73 year-old female with a history of metastatic cholangiocarcinoma presented to the ED with symptoms of progressive productive cough, with sputum described as thin, bright greenish-yellow, and right upper quadrant abdominal pain over a 5-week period. About 18 months prior to presentation, she underwent treatment of the cholangiocarcinoma with systemic chemotherapy and local TARE. Physical exam was notable for productive cough with rhonchi of the right lower lobe. Labs were notable for alkaline phosphatase of 138 IU/L (normal 25-125), and normal AST (13), ALT (10), total bilirubin (0.5). A chest x-ray found no acute abnormality, but a subsequent CT of the chest with contrast revealed hypodense areas around the previous TARE treatment zone. The patient had an endoscopic retrograde cholangiopancreatography performed with a double pigtail stent placement into biloma and BBF. Due to continued bilioptysis, interventional radiology performed a percutaneous transhepatic embolization of the bronchobiliary fistula with coils and an external drain. The patient required 2 additional embolizations before resolution of the BBF.
Discussion: A BBF is a rare, and potentially fatal finding. It is generally associated with liver abscesses, hydatid cysts, malignancies, or trauma. Our patient had development of a BBF approximately 18 months after a TARE procedure for treatment of her cholangiocarcinoma. BBF secondary to TACE has been previously described; however, to our knowledge, this is the first case of BBF secondary to TARE. Treatment options include biliary decompression, such as ERCP and biliary stenting, obliteration of the fistulous tract via embolization, or surgery. Our patient's treatment consisted of stenting via ERCP and percutaneous transhepatic embolization of biliary bronchial fistula on 3 separate occasions. After her first embolization, she achieved significant relief for about 3 weeks. Unfortunately, she developed recurrent bilioptysis and required repeat embolization.

Figure: ERCP with stent placement into biloma with bronchobiliary fistula
Disclosures:
William Green indicated no relevant financial relationships.
Meehir Shah indicated no relevant financial relationships.
William Lippert indicated no relevant financial relationships.
William C. Green, MD, Meehir Shah, MD, William Lippert, MD. B0038 - A Case of Bilioptysis After Transarterial Radioembolization of Primary Cholangiocarcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

