Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0251 - A Rare Entity: Esophageal Dieulafoy Lesion
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- YA
Yasir Ali, MD
Brookdale Hospital Medical Center
Brooklyn, NY
Presenting Author(s)
Yasir Ali, MD1, Muhammad F. Ahmed, MD2, Judah Horowitz, MD2, Rajesh Veluvolu, MD2, Qi Yu, MD3
1Brookdale Hospital Medical Center, Brooklyn, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3NYC Health + Hospitals/King's County, SUNY Downstate, Brookyn, NY
Introduction: Dieulafoy lesions (DL) consist of dilated aberrant submucosal arteries which may potentially lead to life-threatening gastrointestinal (GI) bleeding upon erosion of overlying mucosa. They are most commonly located in the lesser curvature of the stomach followed by duodenum and colon. The esophagus is an exceedingly rare location for DL. We report a hemodynamically unstable patient with distal esophageal DL who presented with massive hematemesis.
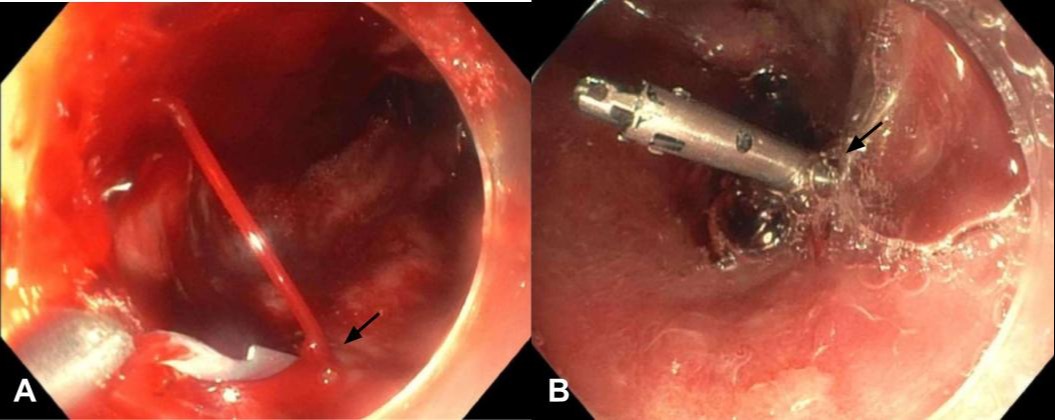
Case Description/Methods: A 57-year-old man was brought to the hospital with massive hematemesis and unresponsiveness requiring intubation in the field. His medical history was significant for alcohol-induced cirrhosis decompensated with ascites. Previous upper endoscopy revealed LA class D esophagitis but no evidence of varices. Upon presentation, the patient was tachycardic to 130 bpm and hypotensive to 89/56 mmHg. Physical exam was remarkable for distended abdomen and positive fluid wave. Initial blood work showed hemoglobin of 4.3 g/dL and platelet of 36/uL. Nasogastric tube suction aspirated 2000 ml of coffee ground content and frank blood. The patient was emergently resuscitated with intravenous fluid and massive transfusion protocol. Subsequently, bedside esophagogastroduodenoscopy revealed active pulsatile bleeding from an exposed vessel in the distal portion of the esophagus [Fig. 1A]. Two hemostatic clips were successfully deployed and hemostasis was achieved [Fig. 1B]. The patient was then transferred to the critical care unit and maintained on proton pump inhibitor infusion. Hospital course was further complicated by hepatic encephalopathy and hepatorenal syndrome. Given MELD-Na score of 40, the patient was eventually transferred to an advanced center for liver transplantation.
Discussion: DL in the esophagus is an extremely rare entity with few cases published to date. Lesions are due to persistently dilated caliber of submucosal artery, as opposed to normal narrowing, as the vessel approaches overlying mucosa. Continuous arterial pulsation may damage the mucosa with a stream of arterial bleeding, as in our case. Upper endoscopy is the mainstay of diagnosis and treatment for DL. Band ligation, electrocautery or hemoclips can be deployed through endoscopy, as with our case. Due to the intermittent nature of bleeding, endoscopy is not always diagnostic and angiography with embolization is an alternative option. Surgery is always a last resort.
Disclosures:
Yasir Ali, MD1, Muhammad F. Ahmed, MD2, Judah Horowitz, MD2, Rajesh Veluvolu, MD2, Qi Yu, MD3. D0251 - A Rare Entity: Esophageal Dieulafoy Lesion, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Brookdale Hospital Medical Center, Brooklyn, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3NYC Health + Hospitals/King's County, SUNY Downstate, Brookyn, NY
Introduction: Dieulafoy lesions (DL) consist of dilated aberrant submucosal arteries which may potentially lead to life-threatening gastrointestinal (GI) bleeding upon erosion of overlying mucosa. They are most commonly located in the lesser curvature of the stomach followed by duodenum and colon. The esophagus is an exceedingly rare location for DL. We report a hemodynamically unstable patient with distal esophageal DL who presented with massive hematemesis.
Case Description/Methods: A 57-year-old man was brought to the hospital with massive hematemesis and unresponsiveness requiring intubation in the field. His medical history was significant for alcohol-induced cirrhosis decompensated with ascites. Previous upper endoscopy revealed LA class D esophagitis but no evidence of varices. Upon presentation, the patient was tachycardic to 130 bpm and hypotensive to 89/56 mmHg. Physical exam was remarkable for distended abdomen and positive fluid wave. Initial blood work showed hemoglobin of 4.3 g/dL and platelet of 36/uL. Nasogastric tube suction aspirated 2000 ml of coffee ground content and frank blood. The patient was emergently resuscitated with intravenous fluid and massive transfusion protocol. Subsequently, bedside esophagogastroduodenoscopy revealed active pulsatile bleeding from an exposed vessel in the distal portion of the esophagus [Fig. 1A]. Two hemostatic clips were successfully deployed and hemostasis was achieved [Fig. 1B]. The patient was then transferred to the critical care unit and maintained on proton pump inhibitor infusion. Hospital course was further complicated by hepatic encephalopathy and hepatorenal syndrome. Given MELD-Na score of 40, the patient was eventually transferred to an advanced center for liver transplantation.
Discussion: DL in the esophagus is an extremely rare entity with few cases published to date. Lesions are due to persistently dilated caliber of submucosal artery, as opposed to normal narrowing, as the vessel approaches overlying mucosa. Continuous arterial pulsation may damage the mucosa with a stream of arterial bleeding, as in our case. Upper endoscopy is the mainstay of diagnosis and treatment for DL. Band ligation, electrocautery or hemoclips can be deployed through endoscopy, as with our case. Due to the intermittent nature of bleeding, endoscopy is not always diagnostic and angiography with embolization is an alternative option. Surgery is always a last resort.
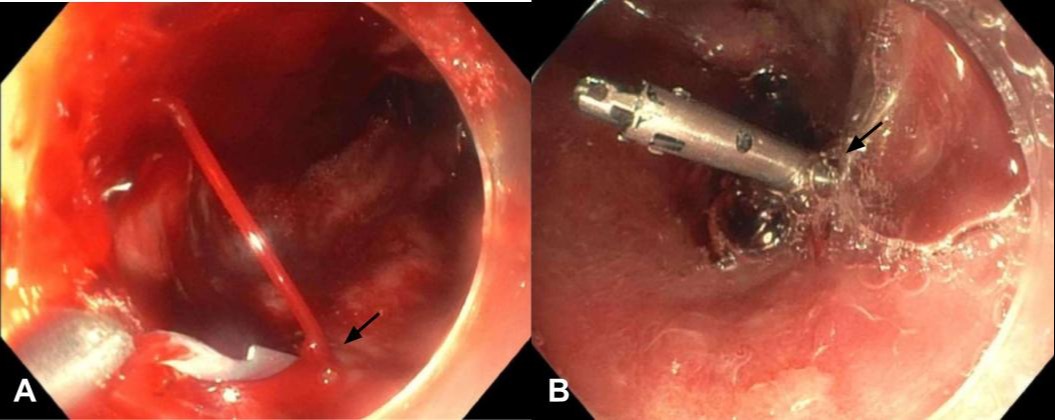
Figure: Figure 1: A) Active pulsatile bleeding from an exposed vessel in the distal portion of the esophagus. B) Hemostatic clip successfully deployed with complete hemostasis
Disclosures:
Yasir Ali indicated no relevant financial relationships.
Muhammad Ahmed indicated no relevant financial relationships.
Judah Horowitz indicated no relevant financial relationships.
Rajesh Veluvolu indicated no relevant financial relationships.
Qi Yu indicated no relevant financial relationships.
Yasir Ali, MD1, Muhammad F. Ahmed, MD2, Judah Horowitz, MD2, Rajesh Veluvolu, MD2, Qi Yu, MD3. D0251 - A Rare Entity: Esophageal Dieulafoy Lesion, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
