Back

Poster Session B - Monday Morning
Category: Esophagus
B0236 - Lymphocytic Esophagitis: A Rare and Rising Cause of Dysphagia
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Ibrar Atiq, MD
United Health Services- Wilson Hospital
Johnson City, NY
Presenting Author(s)
Ibrar Atiq, MD1, Nibir Amin, 2, Usama Sakhawat, MD3, Gowthami Ramar, MD4, Ali Khan, MD4, Nazif Chowdhury, MD4
1United Health Services- Wilson Hospital, Johnson City, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3United Health Services Hospitals, Johnson City, NY; 4United Health Services Hospital, Johnson City, NY
Introduction: Lymphocytic esophagitis (LyE) is a rare esophageal condition with an unknown pathogenesis, prognosis, and limited treatment options. It affects around 0.1% of the population but incidence has been rising. We are presenting a case of lymphocytic esophagitis as a cause of chronic dysphagia, odynophagia and dyspepsia.
Case Description/Methods: An 83-year-old male with a PMH of CAD, HTN, Emphysema, GERD, dysphagia and alcohol use disorder was admitted for worsening dysphagia and generalized weakness for 2 months. The patient reported to have a previous history of dysphagia and underwent esophageal dilation in the past. He described difficulty swallowing that was painful and associated with a burning sensation that recently had worsened after he had stopped taking his PPI a few months prior because of their side effects. In addition, he reported weight loss of 20 lbs over the past few weeks.
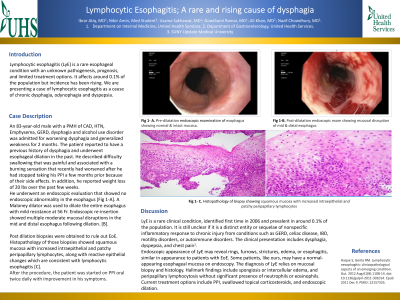
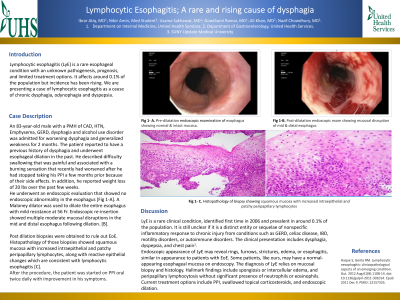
He underwent an endoscopic evaluation that showed no endoscopic abnormality in the esophagus [Fig 1-A]. A Maloney dilator was used to dilate the entire esophagus with mild resistance at 56 Fr. Endoscopic re-insertion showed multiple moderate mucosal disruptions in the mid and distal esophagus following dilation. [B].
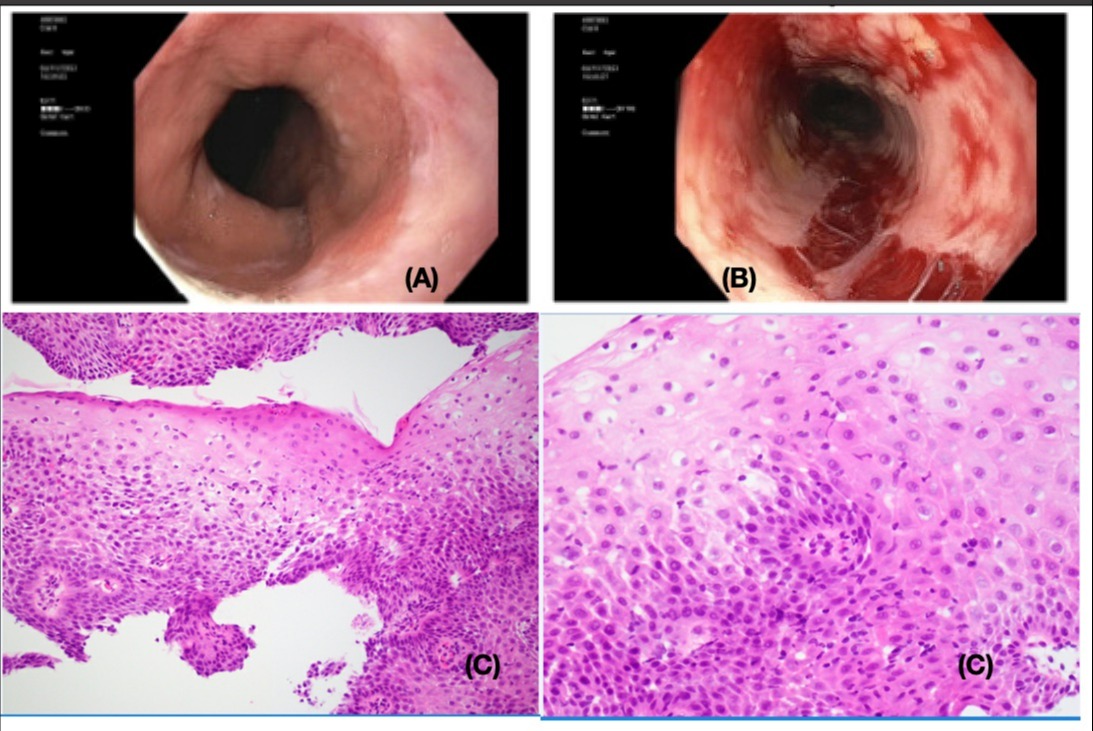
Post dilation biopsies were obtained to rule out EoE. Histopathology of those biopsies showed squamous mucosa with increased intraepithelial and patchy peripapillary lymphocytes, along with reactive epithelial changes which are consistent with lymphocytic esophagitis [C].
After the procedure, the patient was started on PPI oral twice daily with improvement in his symptoms.
Discussion: LyE is a rare clinical condition, identified first time in 2006 and prevalent in around 0.1% of the population. It is still unclear if it is a distinct entity or sequelae of nonspecific inflammatory response to chronic injury from conditions such as GERD, celiac disease, IBD, motility disorders, or autoimmune disorders. The clinical presentation includes dysphagia, dyspepsia, and chest pain.
Endoscopic appearance of LyE may reveal rings, furrows, strictures, edema, or esophagitis, similar in appearance to patients with EoE. Some patients, like ours, may have a normal-appearing esophageal mucosa on endoscopy. The diagnosis of LyE relies on mucosal biopsy and histology. Hallmark findings include spongiosis or intercellular edema, and peripapillary lymphocytosis without significant presence of neutrophils or eosinophils. Current treatment options include PPI, swallowed topical corticosteroids, and endoscopic dilation.
Disclosures:
Ibrar Atiq, MD1, Nibir Amin, 2, Usama Sakhawat, MD3, Gowthami Ramar, MD4, Ali Khan, MD4, Nazif Chowdhury, MD4. B0236 - Lymphocytic Esophagitis: A Rare and Rising Cause of Dysphagia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1United Health Services- Wilson Hospital, Johnson City, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3United Health Services Hospitals, Johnson City, NY; 4United Health Services Hospital, Johnson City, NY
Introduction: Lymphocytic esophagitis (LyE) is a rare esophageal condition with an unknown pathogenesis, prognosis, and limited treatment options. It affects around 0.1% of the population but incidence has been rising. We are presenting a case of lymphocytic esophagitis as a cause of chronic dysphagia, odynophagia and dyspepsia.
Case Description/Methods: An 83-year-old male with a PMH of CAD, HTN, Emphysema, GERD, dysphagia and alcohol use disorder was admitted for worsening dysphagia and generalized weakness for 2 months. The patient reported to have a previous history of dysphagia and underwent esophageal dilation in the past. He described difficulty swallowing that was painful and associated with a burning sensation that recently had worsened after he had stopped taking his PPI a few months prior because of their side effects. In addition, he reported weight loss of 20 lbs over the past few weeks.
He underwent an endoscopic evaluation that showed no endoscopic abnormality in the esophagus [Fig 1-A]. A Maloney dilator was used to dilate the entire esophagus with mild resistance at 56 Fr. Endoscopic re-insertion showed multiple moderate mucosal disruptions in the mid and distal esophagus following dilation. [B].
Post dilation biopsies were obtained to rule out EoE. Histopathology of those biopsies showed squamous mucosa with increased intraepithelial and patchy peripapillary lymphocytes, along with reactive epithelial changes which are consistent with lymphocytic esophagitis [C].
After the procedure, the patient was started on PPI oral twice daily with improvement in his symptoms.
Discussion: LyE is a rare clinical condition, identified first time in 2006 and prevalent in around 0.1% of the population. It is still unclear if it is a distinct entity or sequelae of nonspecific inflammatory response to chronic injury from conditions such as GERD, celiac disease, IBD, motility disorders, or autoimmune disorders. The clinical presentation includes dysphagia, dyspepsia, and chest pain.
Endoscopic appearance of LyE may reveal rings, furrows, strictures, edema, or esophagitis, similar in appearance to patients with EoE. Some patients, like ours, may have a normal-appearing esophageal mucosa on endoscopy. The diagnosis of LyE relies on mucosal biopsy and histology. Hallmark findings include spongiosis or intercellular edema, and peripapillary lymphocytosis without significant presence of neutrophils or eosinophils. Current treatment options include PPI, swallowed topical corticosteroids, and endoscopic dilation.
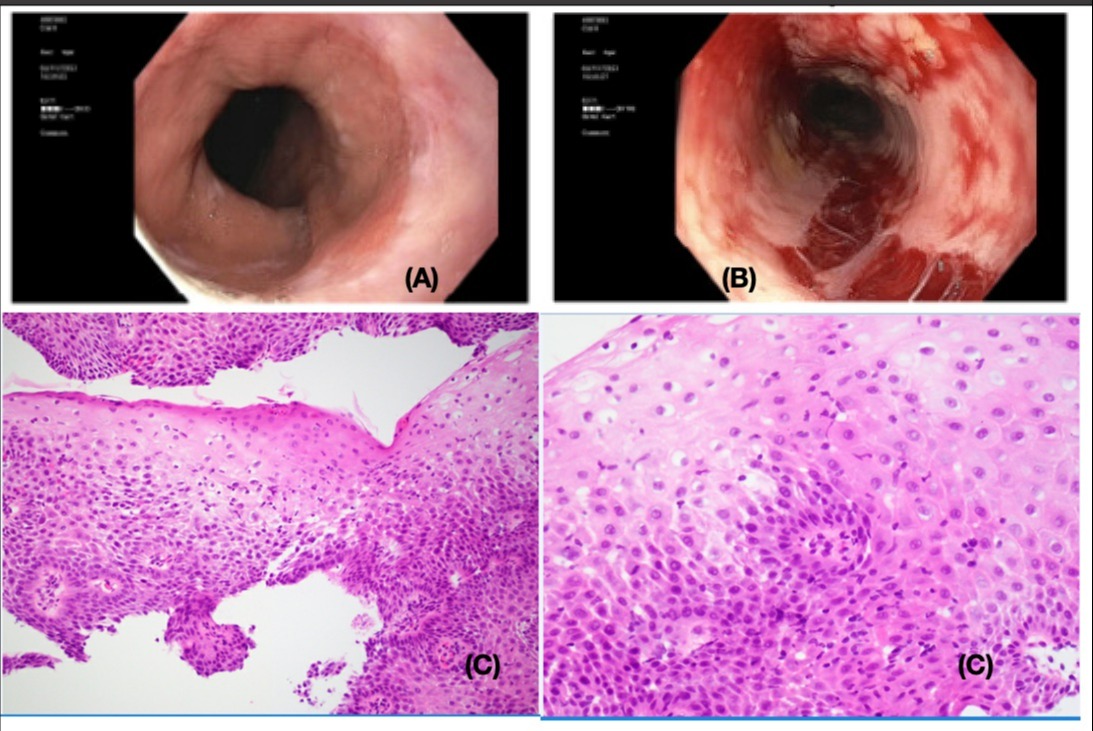
Figure: (A, Pre dilatation esophagus) (B, Post dilatation mucosal disruption of mid & distal esophagus) (C, squamous mucosa with increased intraepithelial and patchy peripapillary lymphocytes)
Disclosures:
Ibrar Atiq indicated no relevant financial relationships.
Nibir Amin indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Gowthami Ramar indicated no relevant financial relationships.
Ali Khan indicated no relevant financial relationships.
Nazif Chowdhury indicated no relevant financial relationships.
Ibrar Atiq, MD1, Nibir Amin, 2, Usama Sakhawat, MD3, Gowthami Ramar, MD4, Ali Khan, MD4, Nazif Chowdhury, MD4. B0236 - Lymphocytic Esophagitis: A Rare and Rising Cause of Dysphagia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
