Back

Poster Session D - Tuesday Morning
Category: Liver
D0530 - All That Is Ammonia Is Not Cirrhosis: A Case of Hyperammonemic Encephalopathy and Anchoring Bias
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Nimish Thakral, MD
University of Kentucky
Pembroke Pines, FL
Presenting Author(s)
Nimish Thakral, MD1, Naba Saeed, MD2, Hammad Qureshi, MD1
1University of Kentucky, Lexington, KY; 2The University of Kentucky, Lexington, KY
Introduction: Anchoring bias is a cognitive bias that results from relying too heavily on the first piece of information that one is provided about a topic. Physicians must make a concerted attempt not to fall prey to anchoring bias as this can lead to a delay in diagnosis and often misdiagnosis. We describe a case of anchoring bias secondary to the diagnosis of hyperammonemic encephalopathy (HAE).
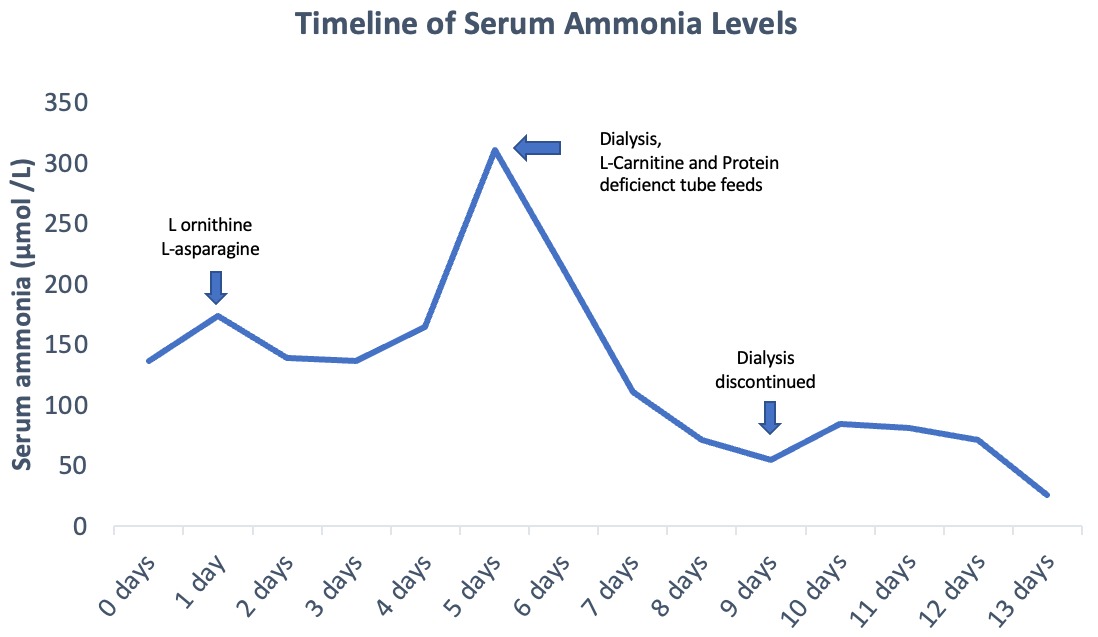
Case Description/Methods: A 20-year-old male with a history of Cerebral Palsy, Cognitive Dysfunction, and Epilepsy, was transferred to our institution secondary to refractory seizures and PEA arrest. Further history entailed gradually worsening mentation with increasing somnolence 3 weeks prior to initial presentation. Initial evaluation revealed elevated venous ammonia of 174 µmol/L. The Hepatology service was consulted for the management of refractory Hepatic Encephalopathy and presumed cirrhosis after the failure of response to lactulose and rifaximin. The addition of L-Ornithine-L-Asparagine had a paradoxical effect with serum ammonia rising to 311µmol/L. Subsequent MRI abdomen and MRCP showed smooth hepatomegaly with no splenomegaly or vascular shunts.
Testing for etiologies of chronic liver disease including Autoimmune Hepatitis, Acute and Chronic viral hepatitis, Cholestatic liver disease, Wilson’s disease, and Alpha-1 antitrypsin deficiency was negative. Plasma amino acids showed elevated Glutamine and Ornithine. Urinary amino acids showed elevated orotic acid. These findings were consistent with Ornithine Aminotransferase deficiency (OAT D). Dialysis was initiated for the rapid reduction of hyperammonemia. The patient responded well to low protein tube feeds and L-Carnitine supplementation with a sustained ammonia reduction after dialysis discontinuation.
Discussion: HAE occurs most commonly in cirrhosis. Other causes include medications, vascular shunts, small intestinal bacterial overgrowth, and inborn errors of metabolism. Our patient likely had OAT D that was unmasked by the recent change in tube feeds. HAE was likely precipitated secondary to the change in feeds and cessation of home bowel regimen due to a self-limited diarrhea episode. OAT D is a rare cause of hyperammonemia which usually presents in the neonatal period but can sometimes be diagnosed in adulthood. In this case, the diagnosis was delayed by anchoring on cirrhosis as a cause for HAE. A high index of suspicion is required to make an accurate diagnosis leading to prompt intervention, thus avoiding delay in care and associated morbidity.
Disclosures:
Nimish Thakral, MD1, Naba Saeed, MD2, Hammad Qureshi, MD1. D0530 - All That Is Ammonia Is Not Cirrhosis: A Case of Hyperammonemic Encephalopathy and Anchoring Bias, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2The University of Kentucky, Lexington, KY
Introduction: Anchoring bias is a cognitive bias that results from relying too heavily on the first piece of information that one is provided about a topic. Physicians must make a concerted attempt not to fall prey to anchoring bias as this can lead to a delay in diagnosis and often misdiagnosis. We describe a case of anchoring bias secondary to the diagnosis of hyperammonemic encephalopathy (HAE).
Case Description/Methods: A 20-year-old male with a history of Cerebral Palsy, Cognitive Dysfunction, and Epilepsy, was transferred to our institution secondary to refractory seizures and PEA arrest. Further history entailed gradually worsening mentation with increasing somnolence 3 weeks prior to initial presentation. Initial evaluation revealed elevated venous ammonia of 174 µmol/L. The Hepatology service was consulted for the management of refractory Hepatic Encephalopathy and presumed cirrhosis after the failure of response to lactulose and rifaximin. The addition of L-Ornithine-L-Asparagine had a paradoxical effect with serum ammonia rising to 311µmol/L. Subsequent MRI abdomen and MRCP showed smooth hepatomegaly with no splenomegaly or vascular shunts.
Testing for etiologies of chronic liver disease including Autoimmune Hepatitis, Acute and Chronic viral hepatitis, Cholestatic liver disease, Wilson’s disease, and Alpha-1 antitrypsin deficiency was negative. Plasma amino acids showed elevated Glutamine and Ornithine. Urinary amino acids showed elevated orotic acid. These findings were consistent with Ornithine Aminotransferase deficiency (OAT D). Dialysis was initiated for the rapid reduction of hyperammonemia. The patient responded well to low protein tube feeds and L-Carnitine supplementation with a sustained ammonia reduction after dialysis discontinuation.
Discussion: HAE occurs most commonly in cirrhosis. Other causes include medications, vascular shunts, small intestinal bacterial overgrowth, and inborn errors of metabolism. Our patient likely had OAT D that was unmasked by the recent change in tube feeds. HAE was likely precipitated secondary to the change in feeds and cessation of home bowel regimen due to a self-limited diarrhea episode. OAT D is a rare cause of hyperammonemia which usually presents in the neonatal period but can sometimes be diagnosed in adulthood. In this case, the diagnosis was delayed by anchoring on cirrhosis as a cause for HAE. A high index of suspicion is required to make an accurate diagnosis leading to prompt intervention, thus avoiding delay in care and associated morbidity.
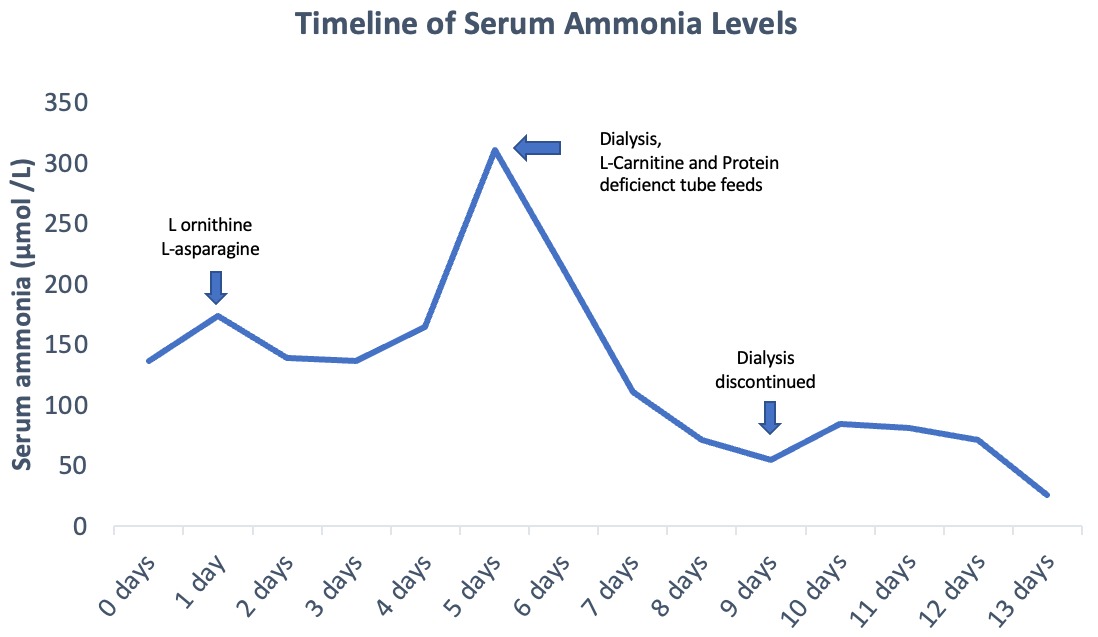
Figure: Timeline of Serum Ammonia Levels
Disclosures:
Nimish Thakral indicated no relevant financial relationships.
Naba Saeed indicated no relevant financial relationships.
Hammad Qureshi indicated no relevant financial relationships.
Nimish Thakral, MD1, Naba Saeed, MD2, Hammad Qureshi, MD1. D0530 - All That Is Ammonia Is Not Cirrhosis: A Case of Hyperammonemic Encephalopathy and Anchoring Bias, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
