Back

Poster Session D - Tuesday Morning
Category: Liver
D0549 - Erdheim-Chester Disease Associated With Aggressive Sclerosing Cholangitis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Ruchi Sharma, MD
University of Iowa Hospital and Carver College of Medicine
Coralville, IA
Presenting Author(s)
Ruchi Sharma, MD1, Mary S. Stone, MD2, Donald E. Macfarlane, MD3, Gopala Koneru, MD3
1University of Iowa Hospital and Carver College of Medicine, Coralville, IA; 2University of Iowa Hospitals and Clinics, Iowa City, IA; 3University of Iowa Hospital and Carver College of Medicine, Iowa City, IA
Introduction: Erdheim-Chester disease (ECD) is a rare histiocytosis recently recognized as a neoplasm due to discovery of MAPK pathway mutations. ECD can involve multiple systems, but hepatic involvement is exceedingly rare.
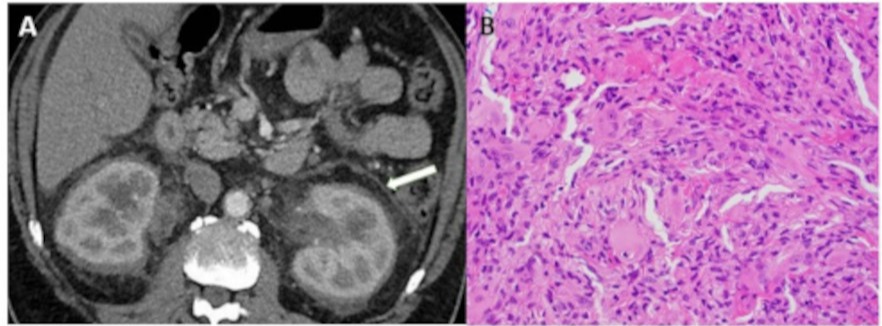
Case Description/Methods: A 64-year-old male presented with fatigue, pruritis, 15-pound weight loss, bilirubin 1.8 mg/dL (0.3-1), and alkaline phosphatase (ALP) 1671 IU/L (44-147). MRCP showed multifocal, short segment dilation of intrahepatic ducts only. Liver biopsy showed periportal and focal bridging fibrosis suggesting primary sclerosing cholangitis (PSC). Anti-smooth muscle, anti-mitochondrial, antineutrophil cytoplasmic antibodies (ANCA) were negative, IgG subclasses normal. A month later he developed emesis, weakness, and leukocytosis. CT scan showed perinephric and periaortic soft tissue stranding suggestive of ECD. 18FDG PET/CT showed a 2.1x2.9 cm highly FDG avid mediastinal mass, follicular lymphoma on biopsy. He improved with antibiotics but returned after a few days with emesis, leukocytosis, and bilirubin 10.7 mg/dL, ALP 1277 IU/L. CT scan showed progressive perinephric and periaortic soft-tissue encasement (Figure1A). Endoscopic retrograde cholangiopancreatography showed a common bile duct (CBD) stricture and non-filling right hepatic duct. Despite CBD stenting bilirubin continued to rise. He now had molluscum like skin lesions which on biopsy revealed dermal proliferation of CD68+, Factor XIIIa+, CD1a- histiocytes and multiple giant cells characteristic of ECD (Figure1B). Targeted therapy with BRAF or MEK pathway inhibitors was considered though there was concern that he may be too sick to receive these. Patient and family opted for comfort care.
Discussion: Despite symptoms, cholestatic liver function and biopsy suggestive of PSC, several factors make us question this diagnosis; such as lack of inflammatory bowel disease or positive ANCA which are seen in 60-80% patients with PSC. PSC is usually indolent, time from diagnosis to death or liver transplant generally being 10-12 years. This patient was transitioned to hospice within 6 months. This makes us suspect hepatic involvement with ECD or an overlap syndrome, or that PSC associated with ECD runs a much more aggressive course. Though liver and CBD biopsies did not show ECD, it is not unusual for biopsy findings in ECD to be obscured by non-specific fibrosis. We want to highlight that a negative biopsy should not delay diagnosis of ECD if imaging is indicative, especially as effective therapy is now available.
Disclosures:
Ruchi Sharma, MD1, Mary S. Stone, MD2, Donald E. Macfarlane, MD3, Gopala Koneru, MD3. D0549 - Erdheim-Chester Disease Associated With Aggressive Sclerosing Cholangitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Iowa Hospital and Carver College of Medicine, Coralville, IA; 2University of Iowa Hospitals and Clinics, Iowa City, IA; 3University of Iowa Hospital and Carver College of Medicine, Iowa City, IA
Introduction: Erdheim-Chester disease (ECD) is a rare histiocytosis recently recognized as a neoplasm due to discovery of MAPK pathway mutations. ECD can involve multiple systems, but hepatic involvement is exceedingly rare.
Case Description/Methods: A 64-year-old male presented with fatigue, pruritis, 15-pound weight loss, bilirubin 1.8 mg/dL (0.3-1), and alkaline phosphatase (ALP) 1671 IU/L (44-147). MRCP showed multifocal, short segment dilation of intrahepatic ducts only. Liver biopsy showed periportal and focal bridging fibrosis suggesting primary sclerosing cholangitis (PSC). Anti-smooth muscle, anti-mitochondrial, antineutrophil cytoplasmic antibodies (ANCA) were negative, IgG subclasses normal. A month later he developed emesis, weakness, and leukocytosis. CT scan showed perinephric and periaortic soft tissue stranding suggestive of ECD. 18FDG PET/CT showed a 2.1x2.9 cm highly FDG avid mediastinal mass, follicular lymphoma on biopsy. He improved with antibiotics but returned after a few days with emesis, leukocytosis, and bilirubin 10.7 mg/dL, ALP 1277 IU/L. CT scan showed progressive perinephric and periaortic soft-tissue encasement (Figure1A). Endoscopic retrograde cholangiopancreatography showed a common bile duct (CBD) stricture and non-filling right hepatic duct. Despite CBD stenting bilirubin continued to rise. He now had molluscum like skin lesions which on biopsy revealed dermal proliferation of CD68+, Factor XIIIa+, CD1a- histiocytes and multiple giant cells characteristic of ECD (Figure1B). Targeted therapy with BRAF or MEK pathway inhibitors was considered though there was concern that he may be too sick to receive these. Patient and family opted for comfort care.
Discussion: Despite symptoms, cholestatic liver function and biopsy suggestive of PSC, several factors make us question this diagnosis; such as lack of inflammatory bowel disease or positive ANCA which are seen in 60-80% patients with PSC. PSC is usually indolent, time from diagnosis to death or liver transplant generally being 10-12 years. This patient was transitioned to hospice within 6 months. This makes us suspect hepatic involvement with ECD or an overlap syndrome, or that PSC associated with ECD runs a much more aggressive course. Though liver and CBD biopsies did not show ECD, it is not unusual for biopsy findings in ECD to be obscured by non-specific fibrosis. We want to highlight that a negative biopsy should not delay diagnosis of ECD if imaging is indicative, especially as effective therapy is now available.
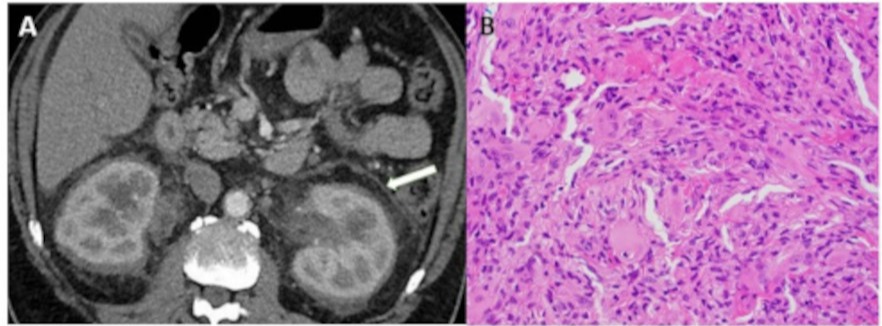
Figure: Figure 1A: CT abdomen showing perinephric soft tissue stranding and encasement. B: extensive histiocytic infiltration (majority of cells) seen on skin biopsy.
Disclosures:
Ruchi Sharma indicated no relevant financial relationships.
Mary Stone indicated no relevant financial relationships.
Donald Macfarlane indicated no relevant financial relationships.
Gopala Koneru indicated no relevant financial relationships.
Ruchi Sharma, MD1, Mary S. Stone, MD2, Donald E. Macfarlane, MD3, Gopala Koneru, MD3. D0549 - Erdheim-Chester Disease Associated With Aggressive Sclerosing Cholangitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
