Back

Poster Session A - Sunday Afternoon
Category: Liver
A0528 - Abdominal Sarcoidosis Including Hepatic and Portal Lymphadenopathy as a Primary Manifestation in a Case of Systemic Sarcoidosis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Saatchi Kuwelker, MD
UT Health San Antonio
San Antonio, TX
Presenting Author(s)
Saatchi Kuwelker, MD1, Farah H. Ladak, MD2, Eugenia Tsai, MD3
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX; 3University of Texas Health Science Center and Texas Liver Institute, San Antonio, TX
Introduction: Sarcoidosis is a rare systemic inflammatory disease characterized by non-caseating granulomas. Most patients are asymptomatic but hepatic sarcoid can progress to portal hypertension which can be cirrhotic or non-cirrhotic. Definitive diagnosis is made by liver biopsy. This is a case of hepatic sarcoidosis presenting with elevation in alkaline phosphatase (ALP) which improved with treatment.
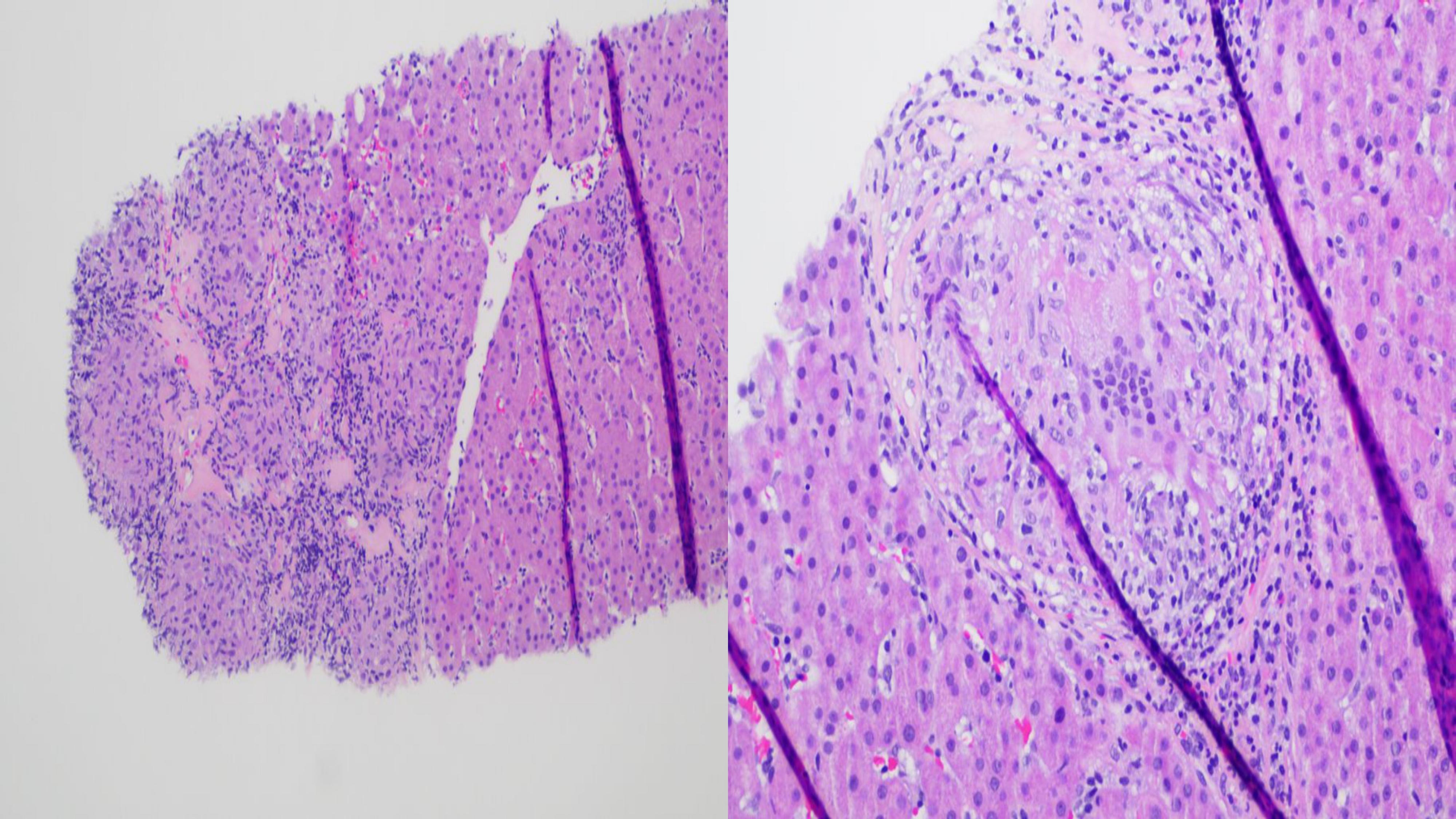
Case Description/Methods: A 50 year-old man presented with three months of worsening dyspnea on exertion and dysphagia to liquids and solids. On arrival, the patient was tachycardic, tachypneic and hypoxemic. Laboratory values revealed an elevated ALP, alanine transaminase (ALT) and aspartate transaminase (AST) of 458 U/L, 113 U/L, 110 U/L, respectively. Computed tomography of the chest showed a small apical pneumothorax and reticular opacities with bronchiectasis. Abdominal ultrasound showed hepatic steatosis. Magnetic resonance cholangiopancreatography of the abdomen revealed enlarged portal lymph nodes. Work-up for fungal, autoimmune and infectious etiologies was negative except for an anti-mitochondrial antibody of 29 units and anti-smooth muscle antibody of 30 units. Liver biopsy revealed granulomatous portal and lobular inflammation, portal lymphocytic inflammation with ductitis, focal interface hepatitis and focal bridging fibrosis (Figure 1). Lung biopsy showed non-necrotizing granulomas that initially was thought to be due to atypical mycobacteria and not sarcoidosis. Therefore, the patient was not immediately started on steroids. Ursodiol was initiated to help with cholestasis. Biopsy of portal lymph nodes confirmed non-caseating granulomas. The patient was then diagnosed with systemic sarcoidosis with hepatic and pulmonary involvement. He was started on steroids in the outpatient setting in conjunction with ursodiol. The AST, ALT, and ALP improved to 50 U/L, 70 U/L and 161 U/L, respectively two months after initiation of therapy.
Discussion: Sarcoidosis should be among one of the differentials in patients presenting with predominant ALP elevation in the absence of bilirubin elevation and concomitant lung manifestations. A liver biopsy is essential for diagnosing hepatic sarcoidosis and to rule out other similar pathologies like primary biliary cholangitis and primary sclerosing cholangitis. Ursodiol in conjunction with steroids can help improve liver enzyme elevations seen in hepatic sarcoidosis.
Disclosures:
Saatchi Kuwelker, MD1, Farah H. Ladak, MD2, Eugenia Tsai, MD3. A0528 - Abdominal Sarcoidosis Including Hepatic and Portal Lymphadenopathy as a Primary Manifestation in a Case of Systemic Sarcoidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX; 3University of Texas Health Science Center and Texas Liver Institute, San Antonio, TX
Introduction: Sarcoidosis is a rare systemic inflammatory disease characterized by non-caseating granulomas. Most patients are asymptomatic but hepatic sarcoid can progress to portal hypertension which can be cirrhotic or non-cirrhotic. Definitive diagnosis is made by liver biopsy. This is a case of hepatic sarcoidosis presenting with elevation in alkaline phosphatase (ALP) which improved with treatment.
Case Description/Methods: A 50 year-old man presented with three months of worsening dyspnea on exertion and dysphagia to liquids and solids. On arrival, the patient was tachycardic, tachypneic and hypoxemic. Laboratory values revealed an elevated ALP, alanine transaminase (ALT) and aspartate transaminase (AST) of 458 U/L, 113 U/L, 110 U/L, respectively. Computed tomography of the chest showed a small apical pneumothorax and reticular opacities with bronchiectasis. Abdominal ultrasound showed hepatic steatosis. Magnetic resonance cholangiopancreatography of the abdomen revealed enlarged portal lymph nodes. Work-up for fungal, autoimmune and infectious etiologies was negative except for an anti-mitochondrial antibody of 29 units and anti-smooth muscle antibody of 30 units. Liver biopsy revealed granulomatous portal and lobular inflammation, portal lymphocytic inflammation with ductitis, focal interface hepatitis and focal bridging fibrosis (Figure 1). Lung biopsy showed non-necrotizing granulomas that initially was thought to be due to atypical mycobacteria and not sarcoidosis. Therefore, the patient was not immediately started on steroids. Ursodiol was initiated to help with cholestasis. Biopsy of portal lymph nodes confirmed non-caseating granulomas. The patient was then diagnosed with systemic sarcoidosis with hepatic and pulmonary involvement. He was started on steroids in the outpatient setting in conjunction with ursodiol. The AST, ALT, and ALP improved to 50 U/L, 70 U/L and 161 U/L, respectively two months after initiation of therapy.
Discussion: Sarcoidosis should be among one of the differentials in patients presenting with predominant ALP elevation in the absence of bilirubin elevation and concomitant lung manifestations. A liver biopsy is essential for diagnosing hepatic sarcoidosis and to rule out other similar pathologies like primary biliary cholangitis and primary sclerosing cholangitis. Ursodiol in conjunction with steroids can help improve liver enzyme elevations seen in hepatic sarcoidosis.
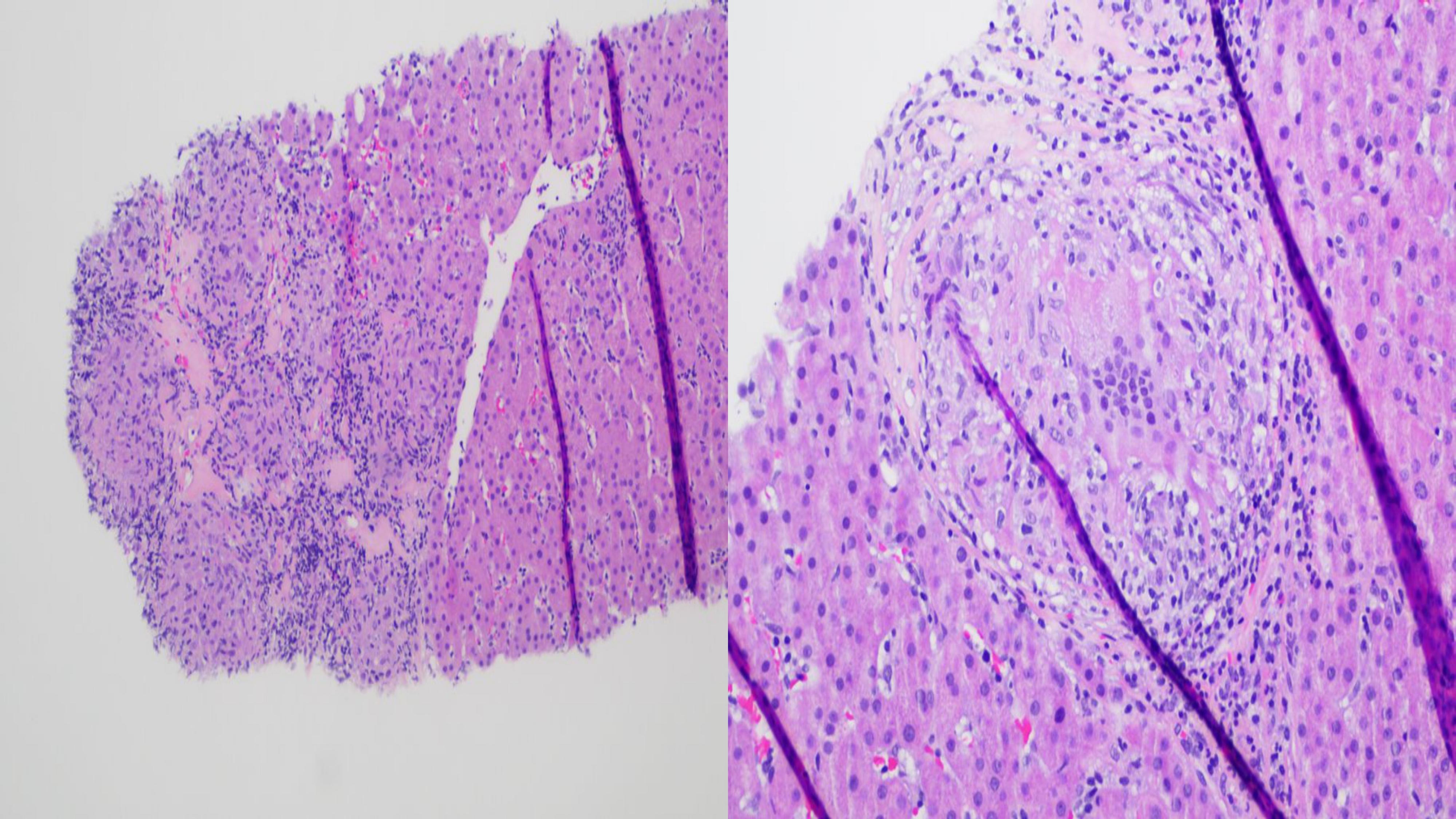
Figure: Figure 1a. Shows a large lobular focus of non-caseating granulomatous inflammation with interdigitating hyaline fibrosis in 200x magnification. The right side of the image shows hepatic parenchyma without steatosis and a small focus of lymphocytic inflammation.
Figure 1b. Shows a higher power image of a portal tract expanded by a poorly formed granuloma with a multinucleated giant cell in 400x magnification. The remaining portal tract shows a lymphohistiocytic infiltrate with infiltration and damage of the bile duct by lymphocytes.
Figure 1b. Shows a higher power image of a portal tract expanded by a poorly formed granuloma with a multinucleated giant cell in 400x magnification. The remaining portal tract shows a lymphohistiocytic infiltrate with infiltration and damage of the bile duct by lymphocytes.
Disclosures:
Saatchi Kuwelker indicated no relevant financial relationships.
Farah Ladak indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Saatchi Kuwelker, MD1, Farah H. Ladak, MD2, Eugenia Tsai, MD3. A0528 - Abdominal Sarcoidosis Including Hepatic and Portal Lymphadenopathy as a Primary Manifestation in a Case of Systemic Sarcoidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
