Back

Poster Session D - Tuesday Morning
Category: Liver
D0585 - Hepatotoxicity From Anabolic Steroids: A Case of Ruptured Liver
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Abigail Bacharach, BS
Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Abbinaya Elangovan, MD1, Abigail Bacharach, BS2, Harry Balanta Murcia, MD1, Seth Sclair, MD1
1University Hospitals Cleveland Medical Center/ Case Western Reserve University, Cleveland, OH; 2Case Western Reserve University, Cleveland, OH
Introduction: Anabolic steroid use can lead to a spectrum of hepatic injuries from abnormal liver function panel to neoplasia. Here we report a middle-aged man who developed a wide range of hepatic manifestations attributable to steroids.
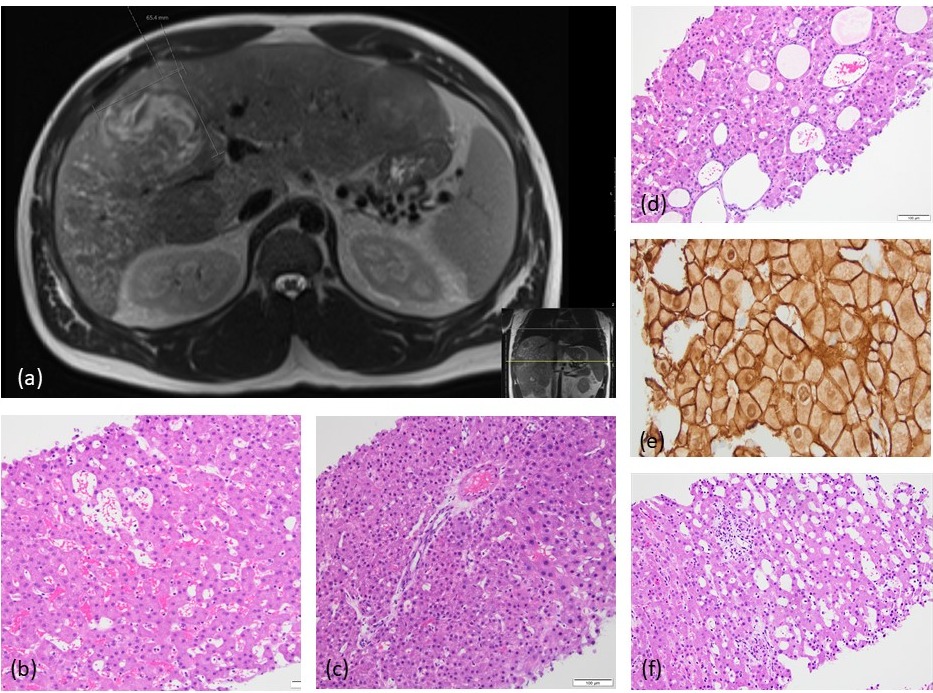
Case Description/Methods: A 30-year-old healthy male presented with six days of fever, right upper quadrant abdominal pain and distension. Social history included 3 years of intravenous anabolic steroid use. On physical exam, he had non-tender hepatomegaly. Labs were remarkable for ALT of 541 U/L, AST of 77 U/L, elevated inflammatory markers, and alpha-fetoprotein < 4. Infectious workup was negative. MRI liver showed enlarged liver (27 cm) with cavernous cystic changes, multiple T2 hyperintense hemorrhagic lesions in the right lobe, the largest measuring 6.8x6.5x7.7 cm, and multiple other hypodense lesions. Random liver biopsy showed areas of sinusoidal dilation, peliosis hepatis, pseudoglandular areas, pseudo portal tracts, and nodular regenerative hyperplasia. Biopsies from hemorrhagic and solid liver masses revealed well-differentiated hepatocellular adenoma which was beta-catenin activated. Malignant transformation could not be excluded in the biopsied liver masses hence surgical resection was recommended. The patient abstained from steroid use however, delayed the surgery due to social reasons. He presented to the hospital four months later with worsening abdominal pain and distension. CT abdomen revealed subcapsular hematoma and hemoperitoneum. He underwent exploratory laparotomy which showed a ruptured hepatic capsule, and a friable right lobe of the liver which had dissected from its ligamentous attachments. He underwent right hepatectomy and resection of adenomas in a staged manner.
Discussion: This case illustrates that anabolic steroids can lead to a spectrum of histological diagnoses in the same patient. Multiple biopsies of the liver with samples inclusive of masses as well as random tissue are crucial. Large adenomas ( >5 cm) have a high risk of malignant transformation and rupture. Pathology after resection is the only way to definitively diagnose or exclude hepatocellular carcinoma (HCC) harboring within adenomatous tissue. Compared to non-users, HCC from steroid users often carries a better prognosis, as it presents earlier in life in the absence of cirrhosis. However, HCC if diagnosed after hepatic rupture, the tumor will be staged metastatic. Hence surgery should be considered in a time-sensitive manner for large adenomas secondary to anabolic steroid use.
Disclosures:
Abbinaya Elangovan, MD1, Abigail Bacharach, BS2, Harry Balanta Murcia, MD1, Seth Sclair, MD1. D0585 - Hepatotoxicity From Anabolic Steroids: A Case of Ruptured Liver, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center/ Case Western Reserve University, Cleveland, OH; 2Case Western Reserve University, Cleveland, OH
Introduction: Anabolic steroid use can lead to a spectrum of hepatic injuries from abnormal liver function panel to neoplasia. Here we report a middle-aged man who developed a wide range of hepatic manifestations attributable to steroids.
Case Description/Methods: A 30-year-old healthy male presented with six days of fever, right upper quadrant abdominal pain and distension. Social history included 3 years of intravenous anabolic steroid use. On physical exam, he had non-tender hepatomegaly. Labs were remarkable for ALT of 541 U/L, AST of 77 U/L, elevated inflammatory markers, and alpha-fetoprotein < 4. Infectious workup was negative. MRI liver showed enlarged liver (27 cm) with cavernous cystic changes, multiple T2 hyperintense hemorrhagic lesions in the right lobe, the largest measuring 6.8x6.5x7.7 cm, and multiple other hypodense lesions. Random liver biopsy showed areas of sinusoidal dilation, peliosis hepatis, pseudoglandular areas, pseudo portal tracts, and nodular regenerative hyperplasia. Biopsies from hemorrhagic and solid liver masses revealed well-differentiated hepatocellular adenoma which was beta-catenin activated. Malignant transformation could not be excluded in the biopsied liver masses hence surgical resection was recommended. The patient abstained from steroid use however, delayed the surgery due to social reasons. He presented to the hospital four months later with worsening abdominal pain and distension. CT abdomen revealed subcapsular hematoma and hemoperitoneum. He underwent exploratory laparotomy which showed a ruptured hepatic capsule, and a friable right lobe of the liver which had dissected from its ligamentous attachments. He underwent right hepatectomy and resection of adenomas in a staged manner.
Discussion: This case illustrates that anabolic steroids can lead to a spectrum of histological diagnoses in the same patient. Multiple biopsies of the liver with samples inclusive of masses as well as random tissue are crucial. Large adenomas ( >5 cm) have a high risk of malignant transformation and rupture. Pathology after resection is the only way to definitively diagnose or exclude hepatocellular carcinoma (HCC) harboring within adenomatous tissue. Compared to non-users, HCC from steroid users often carries a better prognosis, as it presents earlier in life in the absence of cirrhosis. However, HCC if diagnosed after hepatic rupture, the tumor will be staged metastatic. Hence surgery should be considered in a time-sensitive manner for large adenomas secondary to anabolic steroid use.
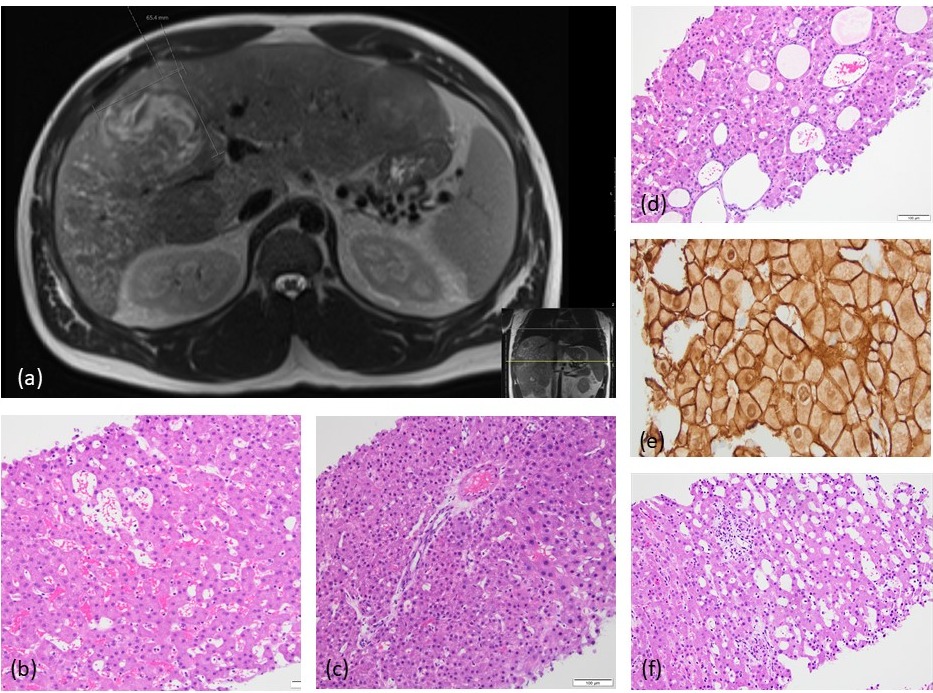
Figure: (a) MRI Liver - cystic changes and adenoma
(b) Peliosis hepatis
(c) Pseudoportal tract
(d) Pseudoglandular area
(e) Abnormal Beta-catenin stain in Hepatic Adenoma
(f) Sinusoidal dilation
(b) Peliosis hepatis
(c) Pseudoportal tract
(d) Pseudoglandular area
(e) Abnormal Beta-catenin stain in Hepatic Adenoma
(f) Sinusoidal dilation
Disclosures:
Abbinaya Elangovan indicated no relevant financial relationships.
Abigail Bacharach indicated no relevant financial relationships.
Harry Balanta Murcia indicated no relevant financial relationships.
Seth Sclair indicated no relevant financial relationships.
Abbinaya Elangovan, MD1, Abigail Bacharach, BS2, Harry Balanta Murcia, MD1, Seth Sclair, MD1. D0585 - Hepatotoxicity From Anabolic Steroids: A Case of Ruptured Liver, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
