Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0027 - Spontaneous Pancreatic Pseudocyst-Superior Mesenteric Vein Fistula: A Case Report
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Spencer Goble, MD
Hennepin County Medical Center (HCMC)
Minneapolis, MN
Presenting Author(s)
Spencer Goble, MD1, Scott Boeke, DO2, Alan Ayoub, 3, Ahmad Malli, MD2
1Hennepin County Medical Center (HCMC), Minneapolis, MN; 2Hennepin County Medical Center (HCMC), University of Minnesota, Minneapolis, MN; 3University of Zagreb Medical School, Minneapolis, MN
Introduction: Fistula development between pancreatic pseudocysts and the portal venous system is a rare and life-threatening complication of acute pancreatitis that is challenging to diagnose and treat. We present this case to highlight certain aspects of diagnosis, management, and potential complications.
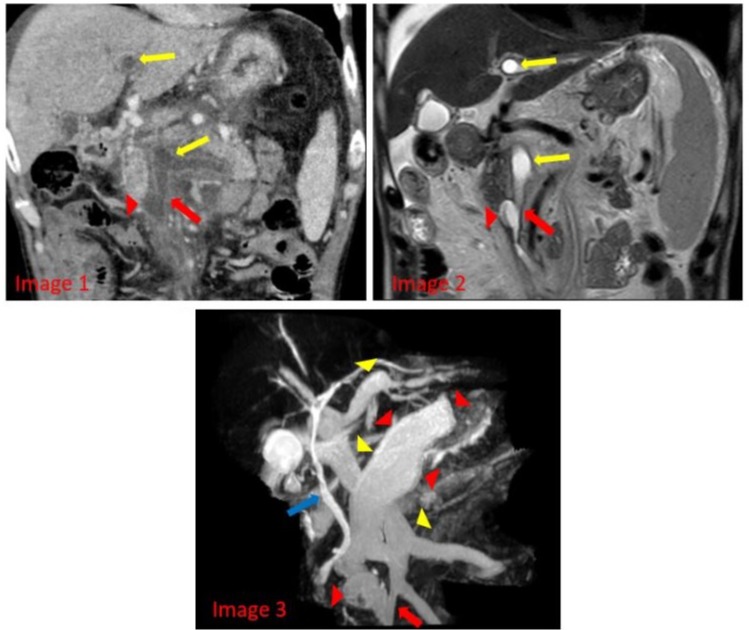
Case Description/Methods: A 50-year-old man with alcohol use disorder presented with 6 months of fatigue, unintentional weight loss, and worsening intermittent abdominal pain. He was diagnosed with acute on chronic pancreatitis based on presentation, labs, and imaging. Contrast-enhanced CT demonstrated diffuse portal venous thrombosis with a questionable fistulous connection between a pancreatic pseudocyst and the portal venous system. A follow-up MRCP revealed a retroperitoneal pseudocyst with an obvious communication with the superior mesenteric and the left portal vein. An ERCP showed a pancreatic duct leak with secondary pancreatic ascites that was managed by pancreatic ductal stenting. Post ERCP course was complicated by septic shock with bacteremia that swiftly resolved with antibiotics. Anticoagulation was deemed inappropriate given the high risk to benefit ratio in the setting of the existing fistula. His course was further complicated by recurrent secondary bacterial and fungal ascites with significant neutrophilia that resolved with antibiotics, pleural effusion requiring brief chest tube placement, and malnutrition that was managed by early enteral nutrition. He gradually improved and was discharged to a rehabilitation facility with stable interval abdominal imaging while on suppressive oral antibiotics.
Discussion: While initial CT raised suspicion for the fistula, MRCP was necessary to make a definitive diagnosis. This is consistent with existing literature that has shown MRCP to be considerably more sensitive than CT. Prompt diagnosis with MRCP and follow up ERCP lead to early pancreatic ductal stenting for management of a pancreatic duct leak with secondary pancreatic ascites, and anticipation of other potential complications (bleeding, infection, and malnutrition) without any need for a surgical intervention.
Considerable complications were seen in this clinical scenario similar to the previously reported literature. Aggressive treatment and anticipation of these complications with accurate imaging, early enteral feeding, pancreatic ductal evaluation, and targeted suppressive antibiotic therapy contributed to the positive outcome on follow up.
Disclosures:
Spencer Goble, MD1, Scott Boeke, DO2, Alan Ayoub, 3, Ahmad Malli, MD2. B0027 - Spontaneous Pancreatic Pseudocyst-Superior Mesenteric Vein Fistula: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Hennepin County Medical Center (HCMC), Minneapolis, MN; 2Hennepin County Medical Center (HCMC), University of Minnesota, Minneapolis, MN; 3University of Zagreb Medical School, Minneapolis, MN
Introduction: Fistula development between pancreatic pseudocysts and the portal venous system is a rare and life-threatening complication of acute pancreatitis that is challenging to diagnose and treat. We present this case to highlight certain aspects of diagnosis, management, and potential complications.
Case Description/Methods: A 50-year-old man with alcohol use disorder presented with 6 months of fatigue, unintentional weight loss, and worsening intermittent abdominal pain. He was diagnosed with acute on chronic pancreatitis based on presentation, labs, and imaging. Contrast-enhanced CT demonstrated diffuse portal venous thrombosis with a questionable fistulous connection between a pancreatic pseudocyst and the portal venous system. A follow-up MRCP revealed a retroperitoneal pseudocyst with an obvious communication with the superior mesenteric and the left portal vein. An ERCP showed a pancreatic duct leak with secondary pancreatic ascites that was managed by pancreatic ductal stenting. Post ERCP course was complicated by septic shock with bacteremia that swiftly resolved with antibiotics. Anticoagulation was deemed inappropriate given the high risk to benefit ratio in the setting of the existing fistula. His course was further complicated by recurrent secondary bacterial and fungal ascites with significant neutrophilia that resolved with antibiotics, pleural effusion requiring brief chest tube placement, and malnutrition that was managed by early enteral nutrition. He gradually improved and was discharged to a rehabilitation facility with stable interval abdominal imaging while on suppressive oral antibiotics.
Discussion: While initial CT raised suspicion for the fistula, MRCP was necessary to make a definitive diagnosis. This is consistent with existing literature that has shown MRCP to be considerably more sensitive than CT. Prompt diagnosis with MRCP and follow up ERCP lead to early pancreatic ductal stenting for management of a pancreatic duct leak with secondary pancreatic ascites, and anticipation of other potential complications (bleeding, infection, and malnutrition) without any need for a surgical intervention.
Considerable complications were seen in this clinical scenario similar to the previously reported literature. Aggressive treatment and anticipation of these complications with accurate imaging, early enteral feeding, pancreatic ductal evaluation, and targeted suppressive antibiotic therapy contributed to the positive outcome on follow up.
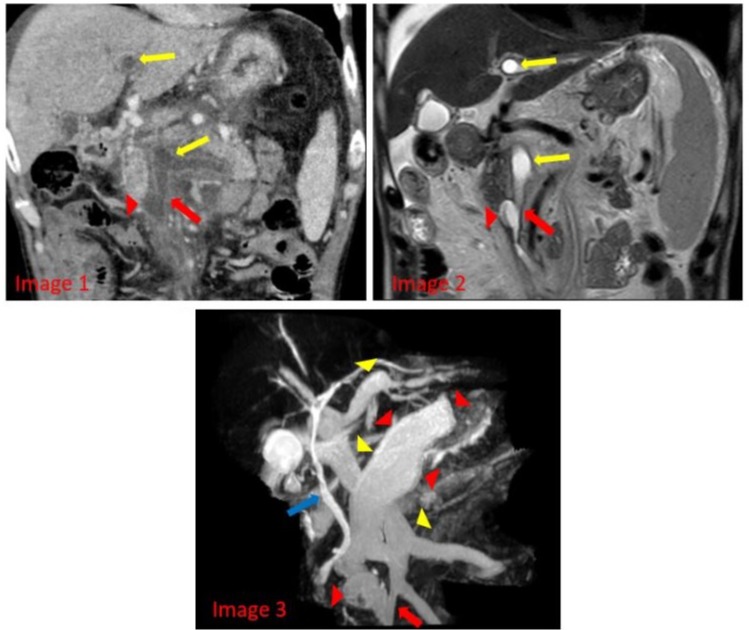
Figure: Images 1 and 2: Coronal CT and T2 weighted MR images, respectively, of the the upper abdomen demonstrate the inferior component of the partially visualized large pseudocyst (red wedge) fistulizing a branch of the SMV near the pancreatic head (red arrow). Fluid density and correlating MR T2 bright fluid signal is noted in the partially visualized proximal SMV and the left portal vein (yellow arrow).
Image 3: MRCP MIP reconstructions are used to emphasize fluid in a 3D image. The large pseudocyst is noted (red wedge) with cystic component fistulizing a branch of the SMV (red arrow). Extension of the pseudocyst conforms to the extrahepatic and intrahepatic portal venous system (yellow wedge). Normal appearing common bile duct also noted (blue arrow).
Image 3: MRCP MIP reconstructions are used to emphasize fluid in a 3D image. The large pseudocyst is noted (red wedge) with cystic component fistulizing a branch of the SMV (red arrow). Extension of the pseudocyst conforms to the extrahepatic and intrahepatic portal venous system (yellow wedge). Normal appearing common bile duct also noted (blue arrow).
Disclosures:
Spencer Goble indicated no relevant financial relationships.
Scott Boeke indicated no relevant financial relationships.
Alan Ayoub indicated no relevant financial relationships.
Ahmad Malli indicated no relevant financial relationships.
Spencer Goble, MD1, Scott Boeke, DO2, Alan Ayoub, 3, Ahmad Malli, MD2. B0027 - Spontaneous Pancreatic Pseudocyst-Superior Mesenteric Vein Fistula: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
