Back

Poster Session C - Monday Afternoon
Category: Esophagus
C0260 - The Dark Side of Drugs: Black Esophagus - A Case Report of Acute Esophageal Necrosis in a Methamphetamine User
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Vinay Jahagirdar, MBBS
University of Missouri Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Daniell Merrill, DO, MBA1, Vinay Jahagirdar, MBBS1, Alisa Likhitsup, MD2
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2Saint Luke's Hospital System, Kansas City, MO
Introduction: Acute esophageal necrosis (AEN) is a severe form of acute esophagitis, visualised endoscopically as dark, black-appearing distal esophageal mucosa. It is a rare finding, with prevalence of 0.01-0.28% of all upper GI endoscopic procedures. Etiology is multifactorial, with tissue hypoperfusion and compromised local protective barriers contributing to necrosis. Patients commonly present with upper GI bleeding. Perforation and stricture formation are important complications. Though direct mortality related to esophageal disease is < 6%, around 1/3rd of patients succumb to the underlying illness.
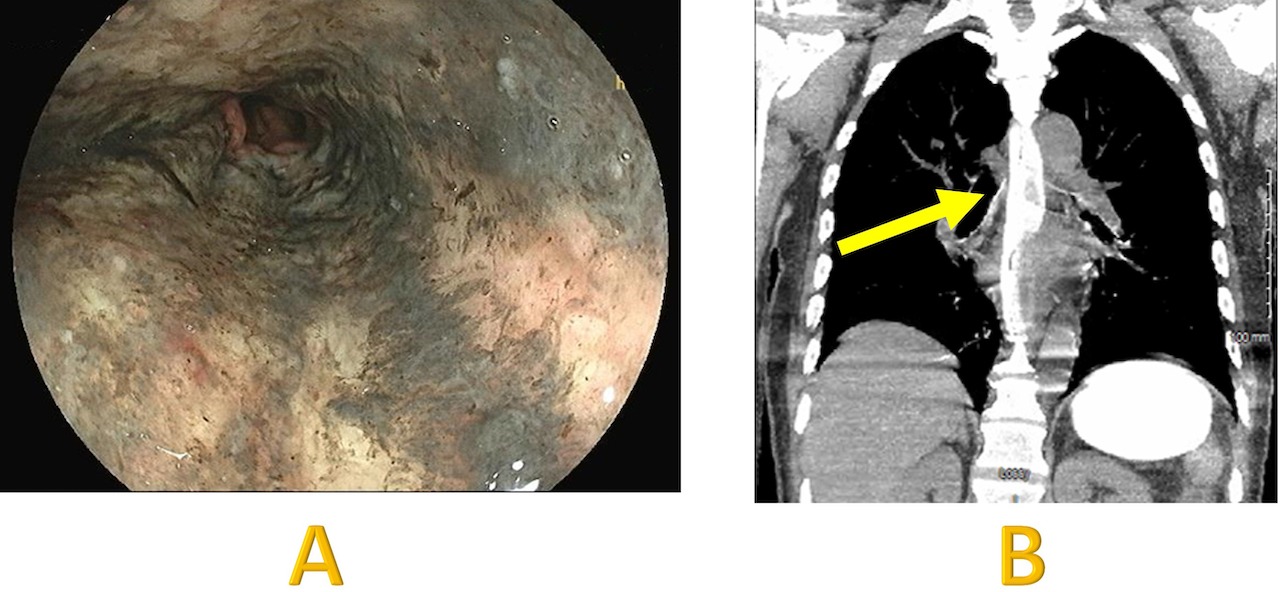
Case Description/Methods: A 60-year-old male with history of polysubstance abuse presented with coffee ground emesis and melena for 10 days. He was found to be in septic shock, respiratory and renal failure. With ongoing hematemesis and agitation, he was intubated emergently, needing two pressors and CRRT. Transaminitis, hypoalbuminemia and coagulopathy were consistent with active alcohol use. UDS was positive for methamphetamine and HCV antibody was detected. With 1.5 L of coffee ground aspirated overnight in the orogastric tube, ocreotide and PPI infusion were initiated with concerns for a variceal bleed. CT chest without contrast showed patulous esophagus with high attenuation enteric contrast material throughout the esophagus. Subsequent EGD revealed circumferential black mucosal discoloration in the esophagus which abruptly stopped at the GE junction, consistent with AEN. A melanotic clot was seen in the fundus but no specific bleeding site was identified. OGT was pulled out. With supportive care, the patient’s improved clinically with time. He was weaned off pressors and extubated on day 7. Blood cultures grew Candida, which was suspected to have translocated from the necrotic esophagus. Micafungin was initiated for candidemia. Patient was discharged on day 16, with referral to substance rehab and hepatology for HCV treatment.
Discussion: Though esophageal necrosis is rare owing to the rich network of collaterals, hemodynamic changes in shock can make the mucosa more vulnerable to ischemia. Mechanical ventilation and vasoactive agents can compound these changes. Though an association has not yet been reported, methamphetamine, a known vasoconstrictor, could have precipitated AEN in our patient. Most cases resolve with standard of care for upper GI bleeding. It is important to avoid nasogastric tubes and maintain NPO status for at least 24 hours to avoid perforation and ensure mucosal healing.
Disclosures:
Daniell Merrill, DO, MBA1, Vinay Jahagirdar, MBBS1, Alisa Likhitsup, MD2. C0260 - The Dark Side of Drugs: Black Esophagus - A Case Report of Acute Esophageal Necrosis in a Methamphetamine User, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2Saint Luke's Hospital System, Kansas City, MO
Introduction: Acute esophageal necrosis (AEN) is a severe form of acute esophagitis, visualised endoscopically as dark, black-appearing distal esophageal mucosa. It is a rare finding, with prevalence of 0.01-0.28% of all upper GI endoscopic procedures. Etiology is multifactorial, with tissue hypoperfusion and compromised local protective barriers contributing to necrosis. Patients commonly present with upper GI bleeding. Perforation and stricture formation are important complications. Though direct mortality related to esophageal disease is < 6%, around 1/3rd of patients succumb to the underlying illness.
Case Description/Methods: A 60-year-old male with history of polysubstance abuse presented with coffee ground emesis and melena for 10 days. He was found to be in septic shock, respiratory and renal failure. With ongoing hematemesis and agitation, he was intubated emergently, needing two pressors and CRRT. Transaminitis, hypoalbuminemia and coagulopathy were consistent with active alcohol use. UDS was positive for methamphetamine and HCV antibody was detected. With 1.5 L of coffee ground aspirated overnight in the orogastric tube, ocreotide and PPI infusion were initiated with concerns for a variceal bleed. CT chest without contrast showed patulous esophagus with high attenuation enteric contrast material throughout the esophagus. Subsequent EGD revealed circumferential black mucosal discoloration in the esophagus which abruptly stopped at the GE junction, consistent with AEN. A melanotic clot was seen in the fundus but no specific bleeding site was identified. OGT was pulled out. With supportive care, the patient’s improved clinically with time. He was weaned off pressors and extubated on day 7. Blood cultures grew Candida, which was suspected to have translocated from the necrotic esophagus. Micafungin was initiated for candidemia. Patient was discharged on day 16, with referral to substance rehab and hepatology for HCV treatment.
Discussion: Though esophageal necrosis is rare owing to the rich network of collaterals, hemodynamic changes in shock can make the mucosa more vulnerable to ischemia. Mechanical ventilation and vasoactive agents can compound these changes. Though an association has not yet been reported, methamphetamine, a known vasoconstrictor, could have precipitated AEN in our patient. Most cases resolve with standard of care for upper GI bleeding. It is important to avoid nasogastric tubes and maintain NPO status for at least 24 hours to avoid perforation and ensure mucosal healing.
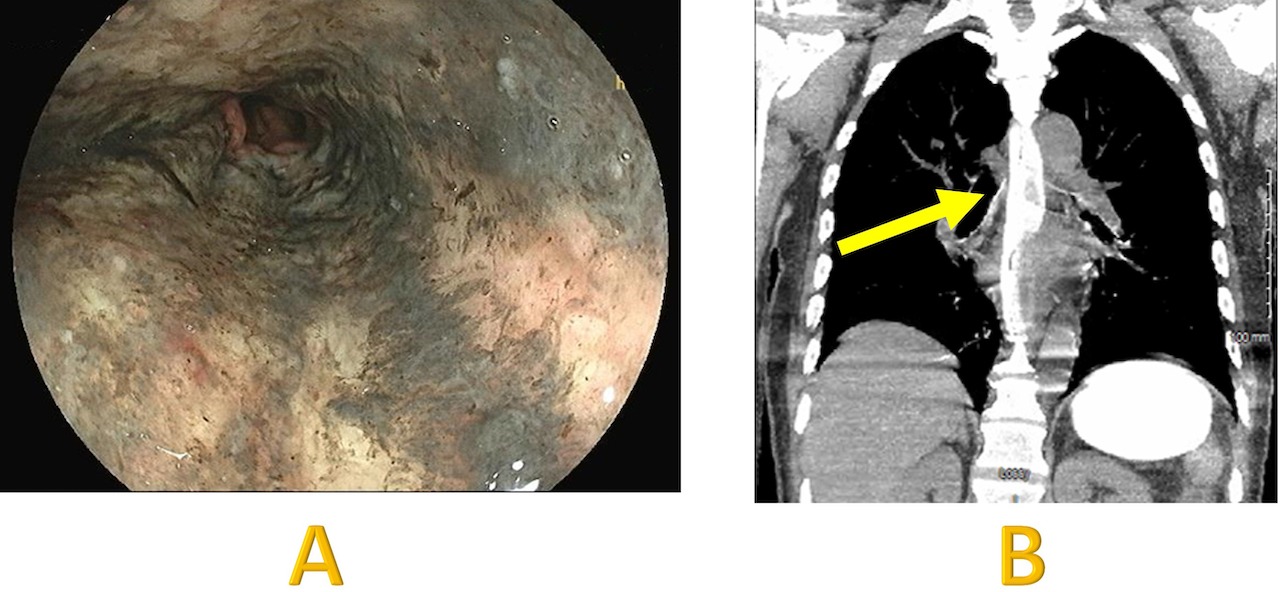
Figure: Image A: EGD showing diffuse circumferential black mucosal discoloration, consistent with AEN. Image B: CT Chest without contrast showing patulous esophagus with high attenuation enteric contrast material throughout the esophagus (arrow).
Disclosures:
Daniell Merrill indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Alisa Likhitsup indicated no relevant financial relationships.
Daniell Merrill, DO, MBA1, Vinay Jahagirdar, MBBS1, Alisa Likhitsup, MD2. C0260 - The Dark Side of Drugs: Black Esophagus - A Case Report of Acute Esophageal Necrosis in a Methamphetamine User, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
