Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0059 - Lower Gastrointestinal Bleeding From a Cystic Artery Pseudoaneurysm in the Setting of Cholecystocolonic Fistula and Gangrenous Cholecystitis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Nishali Shah, BS
Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Nishali Shah, BS1, Mark Bramwit, MD1, Kapil Gupta, MD2, Lea Ann Chen, MD1
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Cholecystocolonic fistula (CCF) is an uncommon complication of cholecystitis in which a tract is formed between the inflamed gallbladder and the colon. CCF are usually asymptomatic and are discovered intraoperatively in < 1% of cholecystectomies.1-2 Herein we discuss an atypical presentation of a CCF.
Case Description/Methods: A 78-year-old male with type II diabetes, coronary artery disease, and a 20 pack-year smoking history presented with two days of progressive hematochezia, dyspnea, and weakness following 6 hours of periumbilical pain. On admission, he was hemodynamically unstable with a blood pressure of 66/34, pulse of 95 BPM, and hemoglobin of 6.2 g/dL.
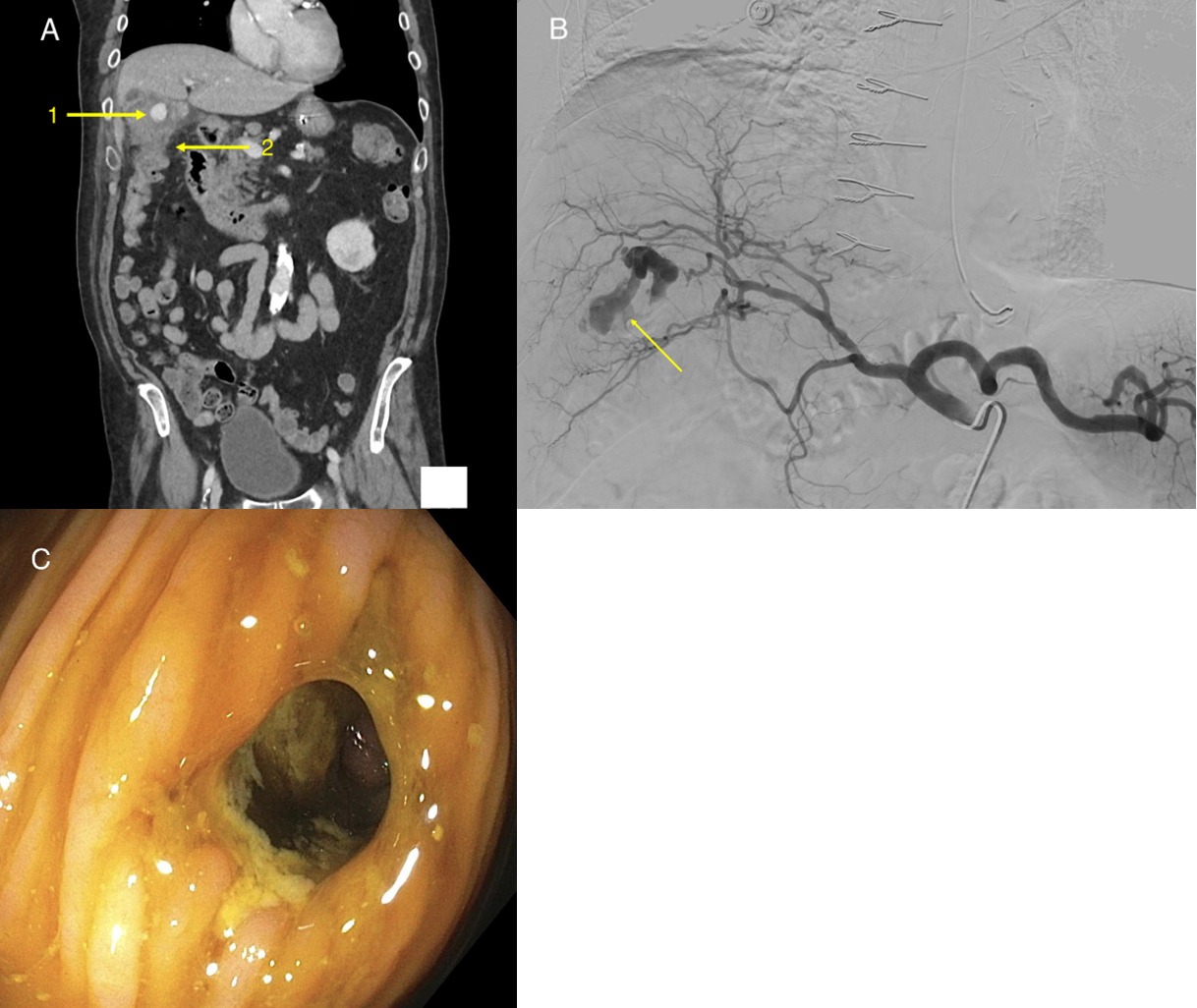
CT abdomen/pelvis revealed an inflamed gallbladder with a hematoma, a pseudoaneurysm (arrow 1), and a CCF to the hepatic flexure (arrow 2) (a). Mesenteric angiogram confirmed a pseudoaneurysm of the cystic artery with active bleeding (b). Colonoscopy confirmed an 8mm circular tract at the hepatic flexure (c). Upper endoscopy was normal.
The patient was diagnosed with gangrenous cholecystitis with CCF and was treated with massive transfusion protocol followed by cystic artery embolization, which successfully halted the hematochezia. The patient was eventually discharged with plans for outpatient cholecystectomy and fistula resection.
Discussion: CCFs are most often found in the setting of biliary disease. The tracts may be formed secondary to stone impaction and subsequent pressure necrosis of the gallbladder lumen in uncomplicated cholecystitis or due to gallbladder wall distension and ischemic necrosis in gangrenous cholecystitis. 85% of these fistulas are found between the gallbladder and duodenum, and only 15% involve the colon.3
CCF is treated with cholecystectomy and fistula resection. While once considered a contraindication to laparoscopic surgery, laparoscopic techniques are now commonly used to treat CCFs with similar success rates and decreased rates of postoperative complications and hospital stays when compared to open procedures.4
Disclosures:
Nishali Shah, BS1, Mark Bramwit, MD1, Kapil Gupta, MD2, Lea Ann Chen, MD1. B0059 - Lower Gastrointestinal Bleeding From a Cystic Artery Pseudoaneurysm in the Setting of Cholecystocolonic Fistula and Gangrenous Cholecystitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Cholecystocolonic fistula (CCF) is an uncommon complication of cholecystitis in which a tract is formed between the inflamed gallbladder and the colon. CCF are usually asymptomatic and are discovered intraoperatively in < 1% of cholecystectomies.1-2 Herein we discuss an atypical presentation of a CCF.
Case Description/Methods: A 78-year-old male with type II diabetes, coronary artery disease, and a 20 pack-year smoking history presented with two days of progressive hematochezia, dyspnea, and weakness following 6 hours of periumbilical pain. On admission, he was hemodynamically unstable with a blood pressure of 66/34, pulse of 95 BPM, and hemoglobin of 6.2 g/dL.
CT abdomen/pelvis revealed an inflamed gallbladder with a hematoma, a pseudoaneurysm (arrow 1), and a CCF to the hepatic flexure (arrow 2) (a). Mesenteric angiogram confirmed a pseudoaneurysm of the cystic artery with active bleeding (b). Colonoscopy confirmed an 8mm circular tract at the hepatic flexure (c). Upper endoscopy was normal.
The patient was diagnosed with gangrenous cholecystitis with CCF and was treated with massive transfusion protocol followed by cystic artery embolization, which successfully halted the hematochezia. The patient was eventually discharged with plans for outpatient cholecystectomy and fistula resection.
Discussion: CCFs are most often found in the setting of biliary disease. The tracts may be formed secondary to stone impaction and subsequent pressure necrosis of the gallbladder lumen in uncomplicated cholecystitis or due to gallbladder wall distension and ischemic necrosis in gangrenous cholecystitis. 85% of these fistulas are found between the gallbladder and duodenum, and only 15% involve the colon.3
CCF is treated with cholecystectomy and fistula resection. While once considered a contraindication to laparoscopic surgery, laparoscopic techniques are now commonly used to treat CCFs with similar success rates and decreased rates of postoperative complications and hospital stays when compared to open procedures.4
- Costi R, et al. CCF: facts and myths. A review of the 231 published cases. J Hepatobiliary Pancreat Surg. 2009. 8-18.
- Tahir OM, et al. Cholecystocolonic fistula. Del Med J. 2014. 373-375.
- Ibrahim IM, et al. Treatment of CCF by laparoscopy. Surg endosc. 1995. 728-729.
- Chowbey PK, et al. Laparoscopic management of cholecystoenteric fistulas. J Laparoendosc Adv Surg Tech. 2006. 467-472.
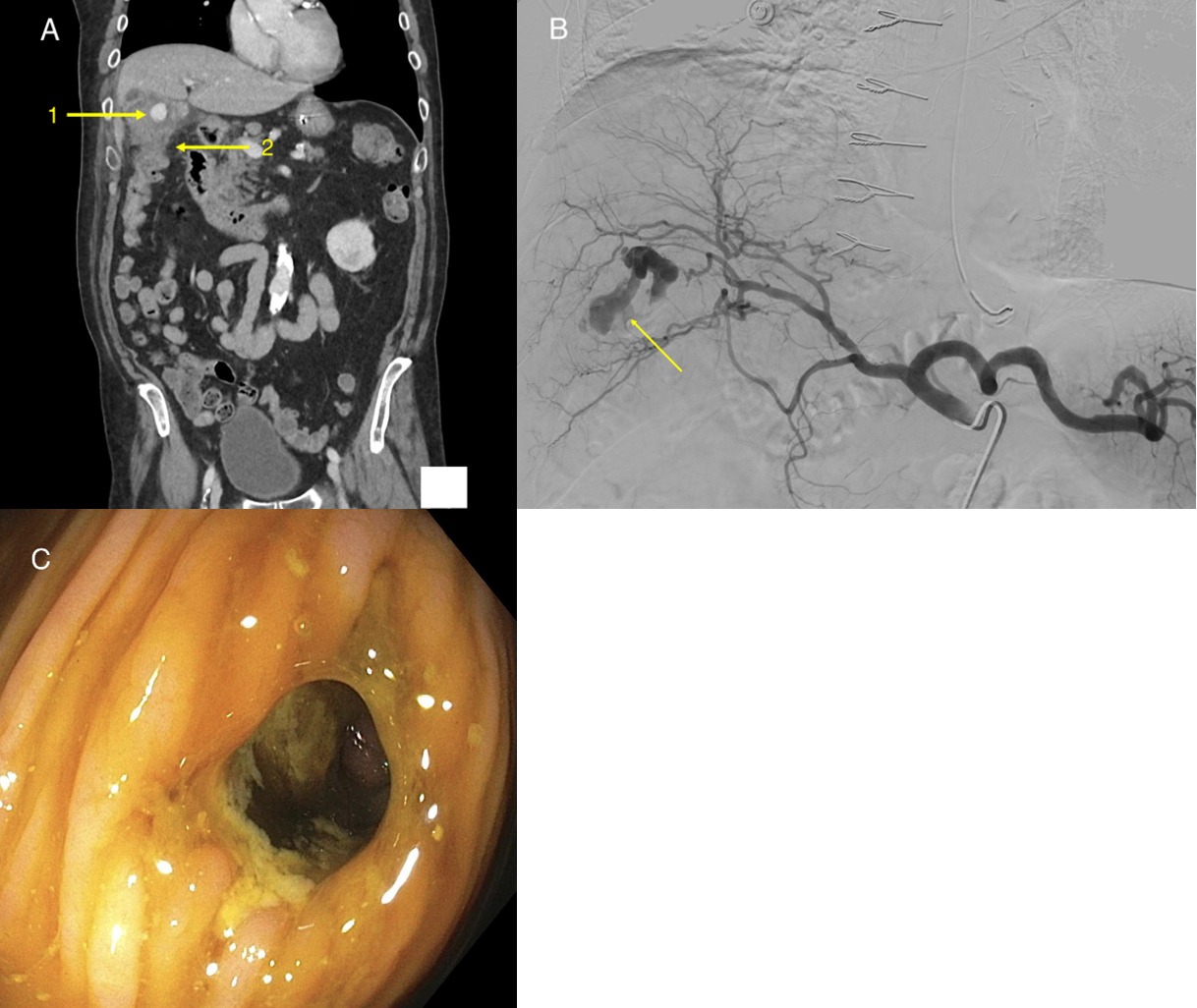
Figure: Contrast enhanced coronal CT scan of the abdomen and pelvis revealed an inflamed gallbladder with a hematoma and pseudoaneurysm (arrow 1) and a fistula from the gallbladder to the hepatic flexure (arrow 2) (a). Mesenteric angiogram confirmed a pseudoaneurysm of the cystic artery with active bleeding (b). Colonoscopy confirmed an 8mm circular tract at the hepatic flexure (c).
Disclosures:
Nishali Shah indicated no relevant financial relationships.
Mark Bramwit indicated no relevant financial relationships.
Kapil Gupta indicated no relevant financial relationships.
Lea Ann Chen: Intrinsic Medicine – Consultant. Phatom – Advisory Committee/Board Member. PredictImmune – Consultant, Grant/Research Support.
Nishali Shah, BS1, Mark Bramwit, MD1, Kapil Gupta, MD2, Lea Ann Chen, MD1. B0059 - Lower Gastrointestinal Bleeding From a Cystic Artery Pseudoaneurysm in the Setting of Cholecystocolonic Fistula and Gangrenous Cholecystitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
