Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0055 - Blame It on the Bamboo Stump: A Pancreatic Ductal Disruption Successfully Managed With Two-Step Endoscopic Therapy
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Aireen Agulto, MD
University of Missouri Health Care
Columbia, MO
Presenting Author(s)
Aireen Agulto, MD1, Faisal Bukeirat, MD1, Harleen K. Chela, MD2, Alhareth Al Juboori, MD1
1University of Missouri Health Care, Columbia, MO; 2University of Missouri-Columbia, Columbia, MO
Introduction: Non-penetrating, isolated pancreatic injuries are rare, and the management is not well-established and challenging. Most injuries are managed by surgery, but recently several case reports discuss endoscopic therapy for treatment of main pancreatic duct disruption. We report a case of pancreatic injury from falling on a bamboo stump with complete pancreatic ductal disruption and complete pancreas divisum with a dominant dorsal duct that was successfully nonoperatively managed through endoscopic therapy.
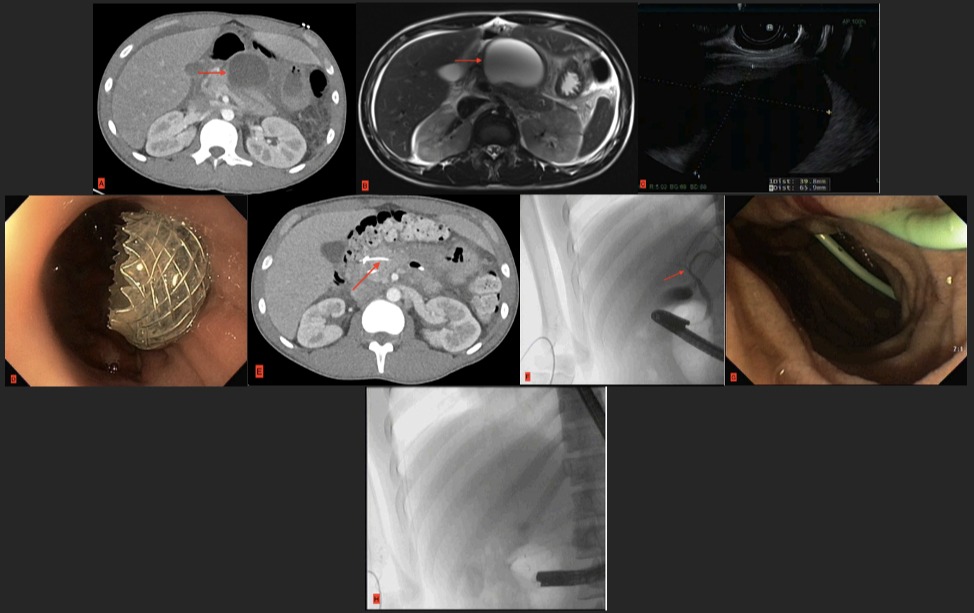
Case Description/Methods: An 18 yo male transferred for worsening abdominal pain from a grade IV pancreatic injury complicated by pancreatic ascites and massive pancreatic fluid collections (PFCs) sustained a month prior after a non-penetrating fall onto a bamboo rod in the Caribbean. He had failed conservative therapy and two attempts with ERCP for pancreatic duct (PD) stent placement. CT A/P and MRCP showed a 13cm cyst consistent with hemorrhagic pancreatic pseudocyst (image A-B). Labs showed leukocytosis, elevated lipase and LFTs, but he was hemodynamically stable. US-guided paracentesis drained 250mL of fluid consistent with pancreatic ascites. To allow for pancreatic edema reduction, we elected for a two-step procedure with separate EUS and ERCP. EUS showed multiple PFCs s/p endoscopic cyst-gastrostomy with Axios stent (image C-D). Repeat CT A/P showed decrease in size of the PFCs (image E). He was discharged and returned in one week for ERCP that revealed a surprising complete pancreas divisum and total disrupted main dorsal PD, which was endoscopically treated with sphincterotomy of the minor papilla and a long PD stent across the disruption (image F-H). The Axios stent was removed a week later, and four weeks later we successfully removed the PD stents from both the major and minor papillae. He made an uneventful recovery and remains well.
Discussion: Pancreatic disruption syndrome or Disconnected Pancreatic Duct Syndrome (DPDS) is an interruption of pancreatic duct continuity, usually from necrotizing pancreatitis, but can occur with blunt or penetrating abdominal injury, as in our patient. Endoscopic management is a minimally invasive option for DPDS and pancreatic ascites. Our patient had severe pancreatic injury managed using two-stage endoscopic therapy, demonstrating a successful treatment strategy for pancreatic injury with total main DPDS. Further studies are required regarding the selection of patients, safety, and long-term outcomes.
Disclosures:
Aireen Agulto, MD1, Faisal Bukeirat, MD1, Harleen K. Chela, MD2, Alhareth Al Juboori, MD1. D0055 - Blame It on the Bamboo Stump: A Pancreatic Ductal Disruption Successfully Managed With Two-Step Endoscopic Therapy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Missouri Health Care, Columbia, MO; 2University of Missouri-Columbia, Columbia, MO
Introduction: Non-penetrating, isolated pancreatic injuries are rare, and the management is not well-established and challenging. Most injuries are managed by surgery, but recently several case reports discuss endoscopic therapy for treatment of main pancreatic duct disruption. We report a case of pancreatic injury from falling on a bamboo stump with complete pancreatic ductal disruption and complete pancreas divisum with a dominant dorsal duct that was successfully nonoperatively managed through endoscopic therapy.
Case Description/Methods: An 18 yo male transferred for worsening abdominal pain from a grade IV pancreatic injury complicated by pancreatic ascites and massive pancreatic fluid collections (PFCs) sustained a month prior after a non-penetrating fall onto a bamboo rod in the Caribbean. He had failed conservative therapy and two attempts with ERCP for pancreatic duct (PD) stent placement. CT A/P and MRCP showed a 13cm cyst consistent with hemorrhagic pancreatic pseudocyst (image A-B). Labs showed leukocytosis, elevated lipase and LFTs, but he was hemodynamically stable. US-guided paracentesis drained 250mL of fluid consistent with pancreatic ascites. To allow for pancreatic edema reduction, we elected for a two-step procedure with separate EUS and ERCP. EUS showed multiple PFCs s/p endoscopic cyst-gastrostomy with Axios stent (image C-D). Repeat CT A/P showed decrease in size of the PFCs (image E). He was discharged and returned in one week for ERCP that revealed a surprising complete pancreas divisum and total disrupted main dorsal PD, which was endoscopically treated with sphincterotomy of the minor papilla and a long PD stent across the disruption (image F-H). The Axios stent was removed a week later, and four weeks later we successfully removed the PD stents from both the major and minor papillae. He made an uneventful recovery and remains well.
Discussion: Pancreatic disruption syndrome or Disconnected Pancreatic Duct Syndrome (DPDS) is an interruption of pancreatic duct continuity, usually from necrotizing pancreatitis, but can occur with blunt or penetrating abdominal injury, as in our patient. Endoscopic management is a minimally invasive option for DPDS and pancreatic ascites. Our patient had severe pancreatic injury managed using two-stage endoscopic therapy, demonstrating a successful treatment strategy for pancreatic injury with total main DPDS. Further studies are required regarding the selection of patients, safety, and long-term outcomes.
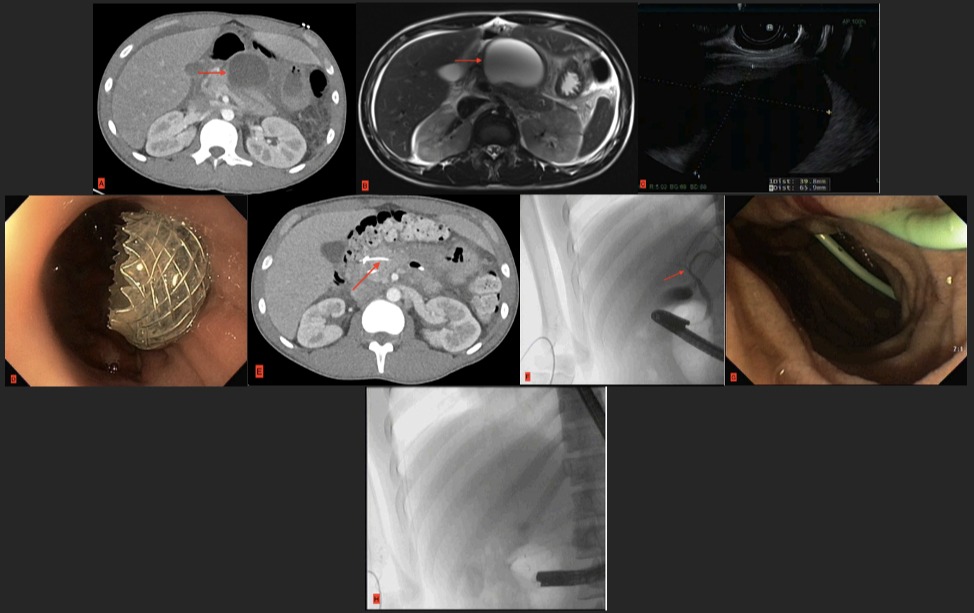
Figure: Image A: CT A/P (coronal) demonstrating edematous pancreas with significant peripancreatic fat stranding, with a peripherally enhancing hypodense fluid collection near the body and tail of the pancreas measuring approximately 4.0 x 4.8 x 13 cm in the maximum AP, RL and SI dimensions (red arrow).
Image B: MRCP (coronal) Abutting the pancreatic body is a multilobulated rim-enhancing complex fluid collection that extends from the level of the diaphragmatic hiatus to just above the level of the aortoiliac bifurcation and measures 6.8 x 9.7 x 19.1 cm (AP by TR by SI, red arrow).
Image C-D: EUS demonstrating large pancreatic fluid collection (PFC, left) and s/p Axios cyst-gastrostomy (right).
Image E: CT A/P (coronal) demonstrating cyst-gastrostomy placement with interval decrease in PFC.
Image F-H: Pancreatogram showed extravastion of contrast material at the junction of proximal 2/3 and distal1/3 of the dorsal PD c/w disrupted dorsal PD (Complete Pancreas divisum, left). Placement of a 5 Fr 9 cm Zimmon PD stent with pigtail crossing the disruption at the minor papilla (center). Pancreatogram showing no extravasation of contrast material s/p PD stent placement.
Image B: MRCP (coronal) Abutting the pancreatic body is a multilobulated rim-enhancing complex fluid collection that extends from the level of the diaphragmatic hiatus to just above the level of the aortoiliac bifurcation and measures 6.8 x 9.7 x 19.1 cm (AP by TR by SI, red arrow).
Image C-D: EUS demonstrating large pancreatic fluid collection (PFC, left) and s/p Axios cyst-gastrostomy (right).
Image E: CT A/P (coronal) demonstrating cyst-gastrostomy placement with interval decrease in PFC.
Image F-H: Pancreatogram showed extravastion of contrast material at the junction of proximal 2/3 and distal1/3 of the dorsal PD c/w disrupted dorsal PD (Complete Pancreas divisum, left). Placement of a 5 Fr 9 cm Zimmon PD stent with pigtail crossing the disruption at the minor papilla (center). Pancreatogram showing no extravasation of contrast material s/p PD stent placement.
Disclosures:
Aireen Agulto indicated no relevant financial relationships.
Faisal Bukeirat indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Alhareth Al Juboori indicated no relevant financial relationships.
Aireen Agulto, MD1, Faisal Bukeirat, MD1, Harleen K. Chela, MD2, Alhareth Al Juboori, MD1. D0055 - Blame It on the Bamboo Stump: A Pancreatic Ductal Disruption Successfully Managed With Two-Step Endoscopic Therapy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
