Back

Poster Session D - Tuesday Morning
Category: Liver
D0606 - Fifteen-Year Evolution of a Rare Hepatic Cystic Lesion: A Case Report
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Anni Chowdhury, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Anni Chowdhury, DO, William Tung, MD, Margaret Skaug, MD, Sreeram Parupudi, MD, FACG
University of Texas Medical Branch, Galveston, TX
Introduction: Hepatic Cysts (HC) are often common incidental findings on Computed Tomography (CT) scans which enlarge silently for years before identification. Here we describe a rare etiology in a patient with hypercoagulable status.
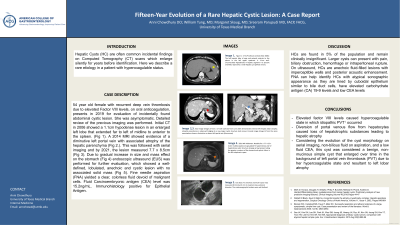
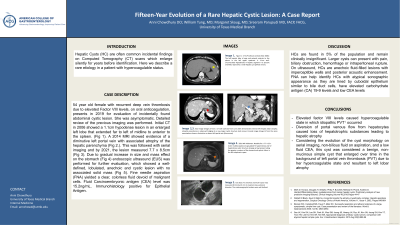
Case Description/Methods: 54 year old female with recurrent deep vein thrombosis due to elevated Factor VIII levels, on oral anticoagulation, presents in 2019 for evaluation of incidentally found abdominal cystic lesion. She was asymptomatic. Detailed review of the previous imaging was performed. Initial CT in 2006 showed a 1.1cm hypodense lesion in an enlarged left lobe that extended far to left of midline to anterior to the spleen. (Fig 1). A 2014 MRI showed evidence of a diminutive left portal vein with associated atrophy of the hepatic parenchyma (Fig 2.). This was followed with serial imaging and by 2021, the lesion measured 7.7 x 8.5cm (Fig 3). Due to gradual increase in size and mass effect on the stomach (Fig 4) endoscopic ultrasound (EUS) was performed for further evaluation, which showed a well-defined, lobulated, anechoic and cystic lesion with no associated solid mass (Fig 5). Fine needle aspiration (FNA) yielded a clear, colorless fluid devoid of malignant cells. Fluid Carcinoembryonic antigen (CEA) level was 15.2ng/mL. Immunohistology positive for Epithelial Antigen.
Discussion: HCs are found in 5% of the population and remain clinically insignificant. Larger cysts can present with pain, biliary obstruction, hemorrhage or intraperitoneal rupture. On ultrasound, HCs are anechoic fluid-filled lesions with imperceptible walls and posterior acoustic enhancement. FNA can help identify HCs with atypical sonographic appearance as they are lined by cuboidal epithelium similar to bile duct cells, have elevated carbohydrate antigen (CA) 19-9 levels and low CEA levels. In this patient, we hypothesize that hepatic atrophy occurred due to portal vein thrombosis(PVT) given that a study showed that elevated factor VIII levels were found in 84% of patients with idiopathic PVT. Additionally, diversion of portal venous flow from hepatocytes causes loss of hepatotrophic substances leading to atrophy as previously reported by Hann et al2. Considering the evolution of the cyst morphology on serial imaging, non-bilious fluid on aspiration, and a low fluid CEA, this cyst was considered a benign, non-mucinous simple cyst that enlarged over time in the background of left portal vein thrombosis (PVT) due to her hypercoagulable state and resultant to left lobar atrophy.

Disclosures:
Anni Chowdhury, DO, William Tung, MD, Margaret Skaug, MD, Sreeram Parupudi, MD, FACG. D0606 - Fifteen-Year Evolution of a Rare Hepatic Cystic Lesion: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Texas Medical Branch, Galveston, TX
Introduction: Hepatic Cysts (HC) are often common incidental findings on Computed Tomography (CT) scans which enlarge silently for years before identification. Here we describe a rare etiology in a patient with hypercoagulable status.
Case Description/Methods: 54 year old female with recurrent deep vein thrombosis due to elevated Factor VIII levels, on oral anticoagulation, presents in 2019 for evaluation of incidentally found abdominal cystic lesion. She was asymptomatic. Detailed review of the previous imaging was performed. Initial CT in 2006 showed a 1.1cm hypodense lesion in an enlarged left lobe that extended far to left of midline to anterior to the spleen. (Fig 1). A 2014 MRI showed evidence of a diminutive left portal vein with associated atrophy of the hepatic parenchyma (Fig 2.). This was followed with serial imaging and by 2021, the lesion measured 7.7 x 8.5cm (Fig 3). Due to gradual increase in size and mass effect on the stomach (Fig 4) endoscopic ultrasound (EUS) was performed for further evaluation, which showed a well-defined, lobulated, anechoic and cystic lesion with no associated solid mass (Fig 5). Fine needle aspiration (FNA) yielded a clear, colorless fluid devoid of malignant cells. Fluid Carcinoembryonic antigen (CEA) level was 15.2ng/mL. Immunohistology positive for Epithelial Antigen.
Discussion: HCs are found in 5% of the population and remain clinically insignificant. Larger cysts can present with pain, biliary obstruction, hemorrhage or intraperitoneal rupture. On ultrasound, HCs are anechoic fluid-filled lesions with imperceptible walls and posterior acoustic enhancement. FNA can help identify HCs with atypical sonographic appearance as they are lined by cuboidal epithelium similar to bile duct cells, have elevated carbohydrate antigen (CA) 19-9 levels and low CEA levels. In this patient, we hypothesize that hepatic atrophy occurred due to portal vein thrombosis(PVT) given that a study showed that elevated factor VIII levels were found in 84% of patients with idiopathic PVT. Additionally, diversion of portal venous flow from hepatocytes causes loss of hepatotrophic substances leading to atrophy as previously reported by Hann et al2. Considering the evolution of the cyst morphology on serial imaging, non-bilious fluid on aspiration, and a low fluid CEA, this cyst was considered a benign, non-mucinous simple cyst that enlarged over time in the background of left portal vein thrombosis (PVT) due to her hypercoagulable state and resultant to left lobar atrophy.

Figure: Left to Right.
Figure 1: CT A/P without contrast (Mar 2006): The left hepatic lobe is large and extends anterior to the spleen in the left upper quadrant. A 1.1cm well-circumscribed hypodensity in hepatic segment II is present and likely represents a small hepatic cyst (yellow arrow).
Figure 2,3: Axial image (Fig 2) from a CT with contrast from June 2014 demonstrates interval left hepatic lobar atrophy; atrophic parenchyma is observed bridging to a now larger cystic structure (red arrow). Coronal image (Fig 3) from the same examination shows a diminutive vs absent left portal vein (blue arrow)
Figure 4: 2021 MRI Abdomen: Notable for a 7.7 x 8.5 x 4.0cm multiloculated, encapsulated T2 hyperintense and T2 hypointense cystic structure (orange arrow) present along the greater curvature of the stomach and splenic hilum in the left subphrenic space
Figure 5: EUS 2022
An anechoic and multi-cystic mass measured 48 mm by 45 mm in maximal cross-sectional diameter. The endosonographic borders were well-defined.
Figure 1: CT A/P without contrast (Mar 2006): The left hepatic lobe is large and extends anterior to the spleen in the left upper quadrant. A 1.1cm well-circumscribed hypodensity in hepatic segment II is present and likely represents a small hepatic cyst (yellow arrow).
Figure 2,3: Axial image (Fig 2) from a CT with contrast from June 2014 demonstrates interval left hepatic lobar atrophy; atrophic parenchyma is observed bridging to a now larger cystic structure (red arrow). Coronal image (Fig 3) from the same examination shows a diminutive vs absent left portal vein (blue arrow)
Figure 4: 2021 MRI Abdomen: Notable for a 7.7 x 8.5 x 4.0cm multiloculated, encapsulated T2 hyperintense and T2 hypointense cystic structure (orange arrow) present along the greater curvature of the stomach and splenic hilum in the left subphrenic space
Figure 5: EUS 2022
An anechoic and multi-cystic mass measured 48 mm by 45 mm in maximal cross-sectional diameter. The endosonographic borders were well-defined.
Disclosures:
Anni Chowdhury indicated no relevant financial relationships.
William Tung indicated no relevant financial relationships.
Margaret Skaug indicated no relevant financial relationships.
Sreeram Parupudi indicated no relevant financial relationships.
Anni Chowdhury, DO, William Tung, MD, Margaret Skaug, MD, Sreeram Parupudi, MD, FACG. D0606 - Fifteen-Year Evolution of a Rare Hepatic Cystic Lesion: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
