Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0075 - Hematochezia Due to Cholecystocolonic Fistula and Gallstone in the Transverse Colon
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Christina Lee, MD
University of Minnesota - Twin Cites, MA
Presenting Author(s)
Christina Lee, MD1, Nicha Wongjarupong, MD2, Robert Matlock, MD3
1University of Minnesota - Twin Cites, Minneapolis, MN; 2University of Minnesota Medical Center, Hennepin County Medical Center, Minneapolis, MN; 3Hennepin County Medical Center (HCMC), Minneapolis, MN
Introduction: We present this case, because cholecystocolonic fistulas are rare, accounting for less than 30% of all cholecystoenteric fistulas. This case emphasizes the unique finding of a rare fistula and the importance of sound clinical judgement for timely diagnosis and follow-up, despite the atypical presentation of the patient.
Case Description/Methods: The patient is a 65-year-old man, with a history of hypertension, hereditary spherocytosis, alcohol-related cirrhosis (MELD-Na of 20) with prior non-bleeding esophageal varices, who presented with hematochezia. He reported three episodes of gross bloody stools for one day, and denied hematemesis and abdominal pain. Seven years prior to this admission, he had a history of choledocholithiasis and presented with painless jaundice. At that time, he underwent an endoscopic retrograde cholangiopancreatography with sphincterotomy and biliary stent placement.
On admission, he was vitally stable. His labs were the following: Hgb 8.3 g/dL (baseline of 12.7 g/dL a year prior to presentation), BUN 6 mg/dL, Cr 0.7 mg/dL, INR 1.4, ALP 108 IU/L, ALT 19 IU/L, AST 41 IU/L, total bilirubin 3.3 mg/dL, and direct bilirubin 1.7 mg/dL.
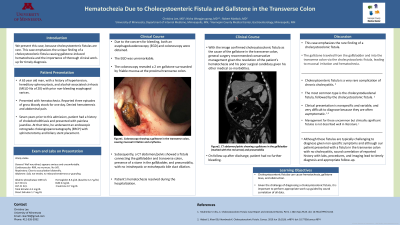
Due to concern for bleeding, both an esophagoduodenoscopy (EGD) and colonoscopy were obtained. The EGD showed portal hypertensive gastropathy without significant source of bleeding. The colonoscopy revealed a 2 cm gallstone surrounded by friable mucosa at the proximal transverse colon. Further work-up with a CT abdomen showed a fistula connecting the gallbladder and transverse colon, presence of a stone in the gallbladder, and pneumobilia, with no intrahepatic or extrahepatic bile duct dilation.
The gallstone lead to mucosal irritation and hematochezia. With the image confirmed cholecystocolonic fistula as the cause of the gallstone in the transverse colon, general surgery recommended conservative management given the resolution of the patient’s hematochezia and his poor surgical candidacy. On follow-up, patient had no further bleeding.
Discussion: Cholecystocolonic fistulas are typically a rare complication of cholelithiasis with cholecystitis, are commonly reported in the sigmoid colon, and commonly lead to gallstone ileus and bleeding. Although these fistulas are typically challenging to diagnose given non-specific symptoms and although our patient presented with a fistula in the transverse colon and no cholecystitis, sound correlation of reported history with labs, procedures, and imaging lead to timely diagnosis and appropriate follow-up.

Disclosures:
Christina Lee, MD1, Nicha Wongjarupong, MD2, Robert Matlock, MD3. A0075 - Hematochezia Due to Cholecystocolonic Fistula and Gallstone in the Transverse Colon, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Minnesota - Twin Cites, Minneapolis, MN; 2University of Minnesota Medical Center, Hennepin County Medical Center, Minneapolis, MN; 3Hennepin County Medical Center (HCMC), Minneapolis, MN
Introduction: We present this case, because cholecystocolonic fistulas are rare, accounting for less than 30% of all cholecystoenteric fistulas. This case emphasizes the unique finding of a rare fistula and the importance of sound clinical judgement for timely diagnosis and follow-up, despite the atypical presentation of the patient.
Case Description/Methods: The patient is a 65-year-old man, with a history of hypertension, hereditary spherocytosis, alcohol-related cirrhosis (MELD-Na of 20) with prior non-bleeding esophageal varices, who presented with hematochezia. He reported three episodes of gross bloody stools for one day, and denied hematemesis and abdominal pain. Seven years prior to this admission, he had a history of choledocholithiasis and presented with painless jaundice. At that time, he underwent an endoscopic retrograde cholangiopancreatography with sphincterotomy and biliary stent placement.
On admission, he was vitally stable. His labs were the following: Hgb 8.3 g/dL (baseline of 12.7 g/dL a year prior to presentation), BUN 6 mg/dL, Cr 0.7 mg/dL, INR 1.4, ALP 108 IU/L, ALT 19 IU/L, AST 41 IU/L, total bilirubin 3.3 mg/dL, and direct bilirubin 1.7 mg/dL.
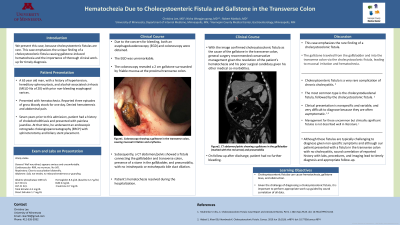
Due to concern for bleeding, both an esophagoduodenoscopy (EGD) and colonoscopy were obtained. The EGD showed portal hypertensive gastropathy without significant source of bleeding. The colonoscopy revealed a 2 cm gallstone surrounded by friable mucosa at the proximal transverse colon. Further work-up with a CT abdomen showed a fistula connecting the gallbladder and transverse colon, presence of a stone in the gallbladder, and pneumobilia, with no intrahepatic or extrahepatic bile duct dilation.
The gallstone lead to mucosal irritation and hematochezia. With the image confirmed cholecystocolonic fistula as the cause of the gallstone in the transverse colon, general surgery recommended conservative management given the resolution of the patient’s hematochezia and his poor surgical candidacy. On follow-up, patient had no further bleeding.
Discussion: Cholecystocolonic fistulas are typically a rare complication of cholelithiasis with cholecystitis, are commonly reported in the sigmoid colon, and commonly lead to gallstone ileus and bleeding. Although these fistulas are typically challenging to diagnose given non-specific symptoms and although our patient presented with a fistula in the transverse colon and no cholecystitis, sound correlation of reported history with labs, procedures, and imaging lead to timely diagnosis and appropriate follow-up.

Figure: Figure 1. The CT abdomen and pelvis shows the area of the cholecystocolonic fistula with gallstone in the gallbladder (both marked with red arrow), and pneumobilia.
Disclosures:
Christina Lee indicated no relevant financial relationships.
Nicha Wongjarupong indicated no relevant financial relationships.
Robert Matlock indicated no relevant financial relationships.
Christina Lee, MD1, Nicha Wongjarupong, MD2, Robert Matlock, MD3. A0075 - Hematochezia Due to Cholecystocolonic Fistula and Gallstone in the Transverse Colon, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
