Back

Poster Session D - Tuesday Morning
Category: Practice Management
D0618 - Improving First-case On-time Procedure Starts in a Large Health Care Network
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- NM
Noel Bernard Martins, MD
St. Luke's University Health Network
Fountain Hill, PA
Presenting Author(s)
Noel Martins, MD1, Hussam Tayel, MD1, Brian Kim, DO1, Lynette Colaco Martins, LLB, MBe, LLM2, Yecheskel Schneider, MD1, Paul Dumitrescu, BS3, Matthew Record, BA3, Scott Siegfried, 1, Cynthia Anthony, 1
1St. Luke's University Health Network, Bethlehem, PA; 2Yale Law School Solomon Center for Health Law and Policy, New Haven, CT; 3Temple University School of Medicine, Bethlehem, PA
Introduction: Delays in the endoscopy unit procedure room can lead to provider, staff, and patient dissatisfaction, and increased costs. Starting the first-case on-time can reduce these delays, improve efficiency, and improve provider and staff morale, and patient satisfaction. At baseline, our first-cases only started on time 78.4% of the time and the a reason was often not given for delays. Our goals were to increase our first-case on-time start rate to more than 90% and increase how often a reason was given for a late start to more than 90%.
Methods: We included data for the 35 employed Gastroenterologists in our network. We excluded late starts due to patient, staff, facility, anesthesia, or change in case order. Our first intervention took place at the end of 10/2021 and included a presentation to our Gastroenterologists at a Department Meeting and then monthly emails to all Gastroenterologists with all Gastroenterologists' first-case on-time start rate. Our second intervention took place on 1/11/2022 and involved adding a hard-stop so an endoscopy nurse was forced to select a reason for every late first-case start. We continued to collect our data from 11/1/2021 to 1/10/2022 (after the first intervention) and from 1/11/2022 to 5/31/2022 (after the second intervention). We also tracked how often a reason was given for a late start. We used a Chi Square test to compare the rates before and after the first intervention, and then before and after the second intervention.
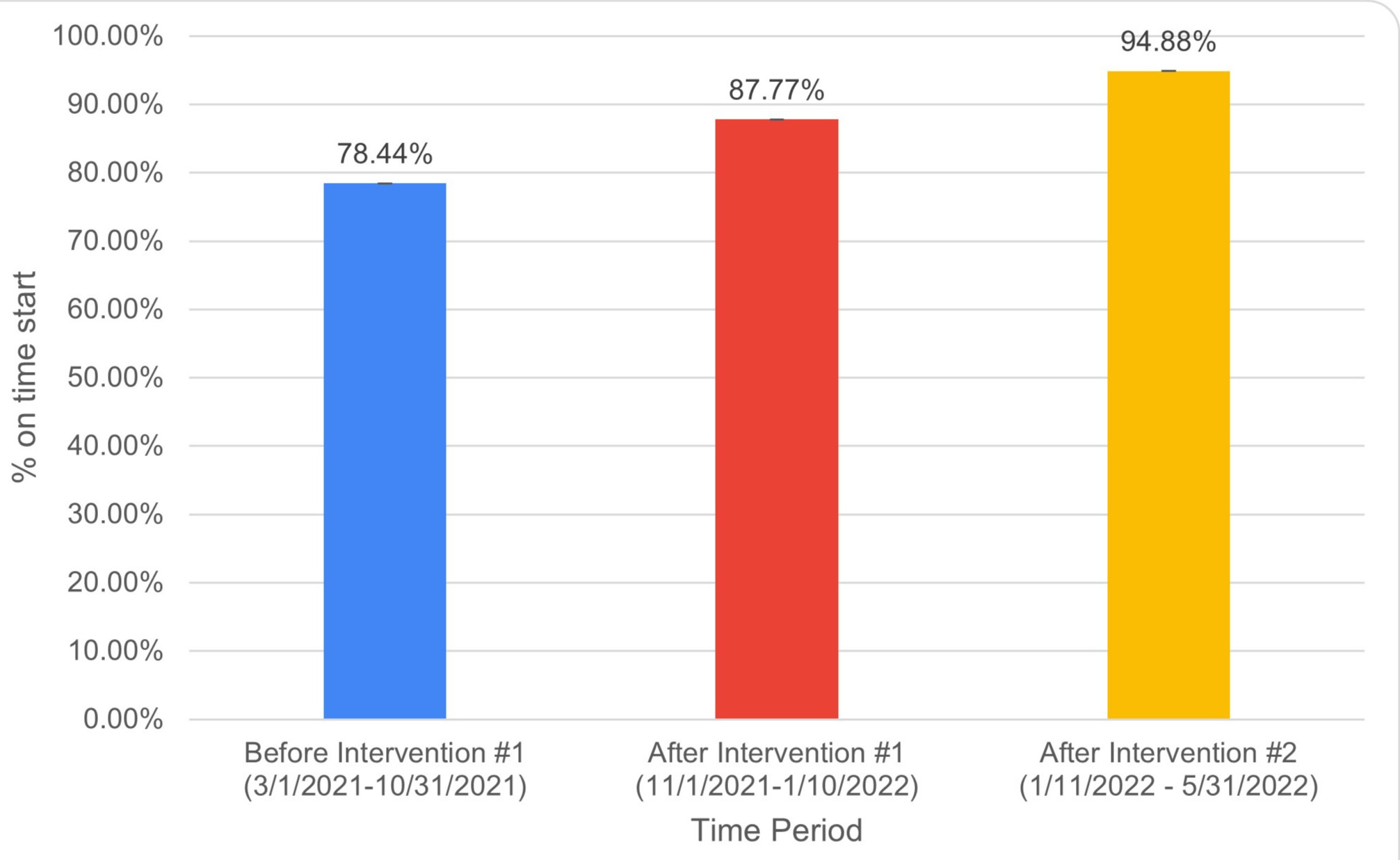
Results: The first-case on-time start rate increased from 1695/2161 (78.4%) to 531/605 (87.8%) after the first intervention (p< 0.00001). It then increased to 1242/1309 (94.9%) after the second intervention (p< 0.00001). The frequency of how often a reason was given for a late start increased from 120/540 (22.2%) to 53/67 (79.1%) after the hard-stop was added on 1/11/2022 (p< 0.00001).
Discussion: These two interventions led to a significant increase in our first-case on-time start rate and how often a reason was given for a late start. This underscores the importance of regular feedback about start times as our Gastroenterologists were more motivated to start on-time when they knew their rates would be emailed to the rest of the group. Now that we are collecting data for the majority of late starts, we are able to use this data to focus on the reasons for the remaining late starts. There have been discussions about adding this hard-stop in the operating room to improve the quality of the data we collect there as well.
Disclosures:
Noel Martins, MD1, Hussam Tayel, MD1, Brian Kim, DO1, Lynette Colaco Martins, LLB, MBe, LLM2, Yecheskel Schneider, MD1, Paul Dumitrescu, BS3, Matthew Record, BA3, Scott Siegfried, 1, Cynthia Anthony, 1. D0618 - Improving First-case On-time Procedure Starts in a Large Health Care Network, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2Yale Law School Solomon Center for Health Law and Policy, New Haven, CT; 3Temple University School of Medicine, Bethlehem, PA
Introduction: Delays in the endoscopy unit procedure room can lead to provider, staff, and patient dissatisfaction, and increased costs. Starting the first-case on-time can reduce these delays, improve efficiency, and improve provider and staff morale, and patient satisfaction. At baseline, our first-cases only started on time 78.4% of the time and the a reason was often not given for delays. Our goals were to increase our first-case on-time start rate to more than 90% and increase how often a reason was given for a late start to more than 90%.
Methods: We included data for the 35 employed Gastroenterologists in our network. We excluded late starts due to patient, staff, facility, anesthesia, or change in case order. Our first intervention took place at the end of 10/2021 and included a presentation to our Gastroenterologists at a Department Meeting and then monthly emails to all Gastroenterologists with all Gastroenterologists' first-case on-time start rate. Our second intervention took place on 1/11/2022 and involved adding a hard-stop so an endoscopy nurse was forced to select a reason for every late first-case start. We continued to collect our data from 11/1/2021 to 1/10/2022 (after the first intervention) and from 1/11/2022 to 5/31/2022 (after the second intervention). We also tracked how often a reason was given for a late start. We used a Chi Square test to compare the rates before and after the first intervention, and then before and after the second intervention.
Results: The first-case on-time start rate increased from 1695/2161 (78.4%) to 531/605 (87.8%) after the first intervention (p< 0.00001). It then increased to 1242/1309 (94.9%) after the second intervention (p< 0.00001). The frequency of how often a reason was given for a late start increased from 120/540 (22.2%) to 53/67 (79.1%) after the hard-stop was added on 1/11/2022 (p< 0.00001).
Discussion: These two interventions led to a significant increase in our first-case on-time start rate and how often a reason was given for a late start. This underscores the importance of regular feedback about start times as our Gastroenterologists were more motivated to start on-time when they knew their rates would be emailed to the rest of the group. Now that we are collecting data for the majority of late starts, we are able to use this data to focus on the reasons for the remaining late starts. There have been discussions about adding this hard-stop in the operating room to improve the quality of the data we collect there as well.
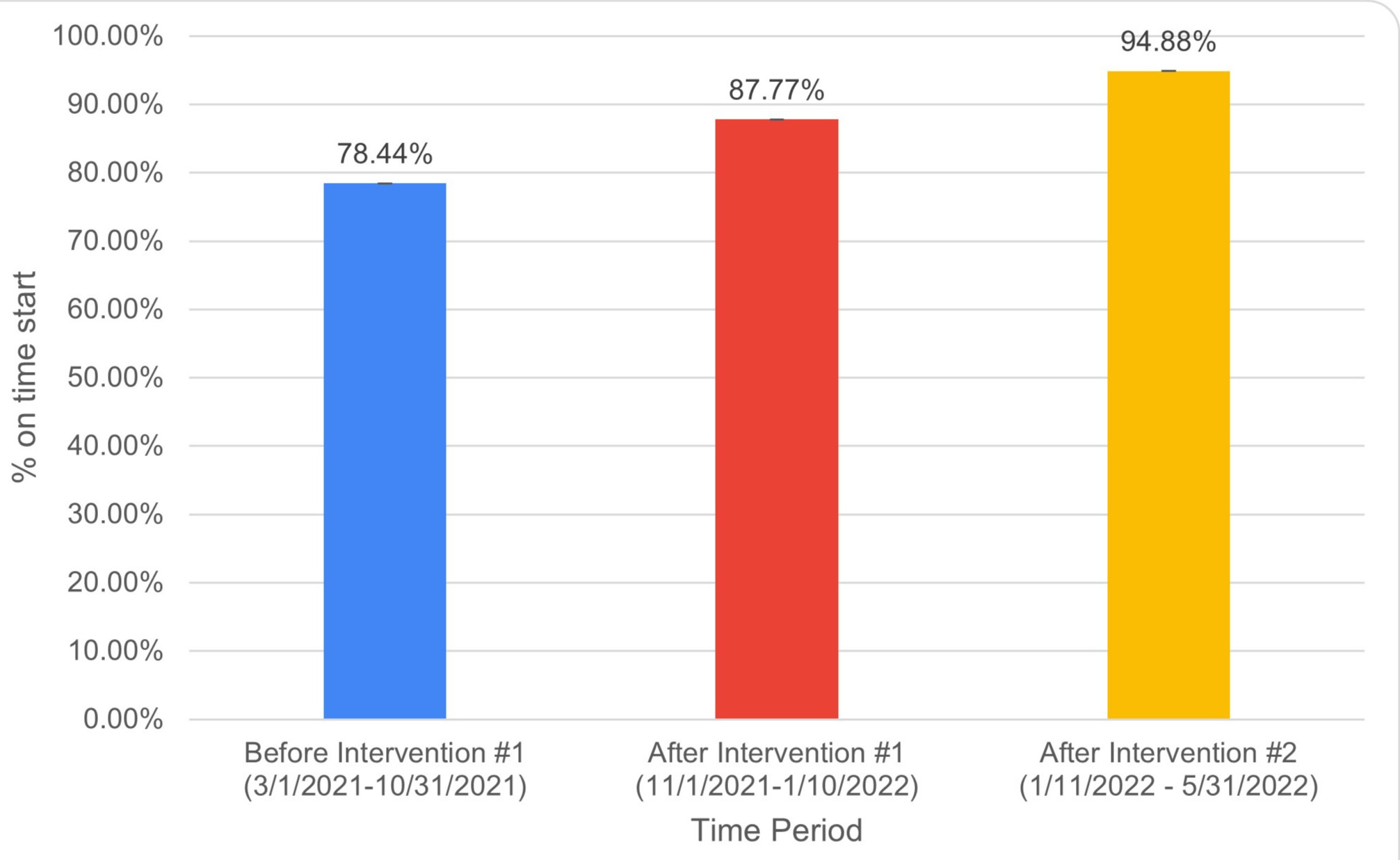
Figure: Increase in first-case on-time procedure starts after the first and second interventions.
Disclosures:
Noel Martins indicated no relevant financial relationships.
Hussam Tayel indicated no relevant financial relationships.
Brian Kim indicated no relevant financial relationships.
Lynette Colaco Martins indicated no relevant financial relationships.
Yecheskel Schneider indicated no relevant financial relationships.
Paul Dumitrescu indicated no relevant financial relationships.
Matthew Record indicated no relevant financial relationships.
Scott Siegfried indicated no relevant financial relationships.
Cynthia Anthony indicated no relevant financial relationships.
Noel Martins, MD1, Hussam Tayel, MD1, Brian Kim, DO1, Lynette Colaco Martins, LLB, MBe, LLM2, Yecheskel Schneider, MD1, Paul Dumitrescu, BS3, Matthew Record, BA3, Scott Siegfried, 1, Cynthia Anthony, 1. D0618 - Improving First-case On-time Procedure Starts in a Large Health Care Network, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

