Back

Poster Session D - Tuesday Morning
Category: Practice Management
D0619 - Efficacy of a Curriculum Teaching Healthcare Disparities in Gastroenterology Fellowship
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Natalie Mitchell, MD
Brooke Army Medical Center
San Antonio, Texas
Presenting Author(s)
Natalie Mitchell, MD1, Sarah Ordway, MD2, Ross Humes, MD3, Manish Singla, MD4
1Brooke Army Medical Center, San Antonio, TX; 2Carl R. Darnall Army Medical Center, Fort Hood, TX; 3Dwight D. Eisenhower Army Medical Center, Fort Gordon, GA; 4Capital Digestive Care, Chevy Chase, MD
Introduction: There are many studies identifying healthcare disparities based on sex, race, and economic status in gastroenterology (GI) influenced by the social determinants of health. The Accreditation Council for Graduate Medical Education (ACGME) recently mandated that medical training programs provide education about healthcare disparities. Tools to provide this education are lacking, and methods to address health equity remain unfamiliar to many health care systems, their leaders, and medical educators. The aim of this study was to pilot a healthcare disparities curriculum for our GI fellowship program.
Methods: Using the Kern 6-step method, we designed a year-long health disparities curriculum and implemented it in our GI fellowship from 2020-2021. During weekly academics, a fellow presented a journal article identifying a disparity in GI followed by guided group discussion about how to apply that study to our own practice and patient population. We developed a validated survey to assess knowledge and attitudes about healthcare disparities before and after implementation of the curriculum.
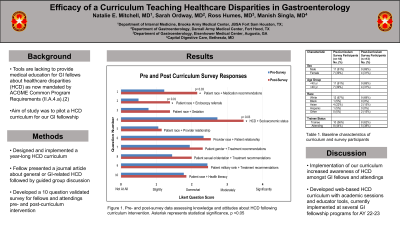
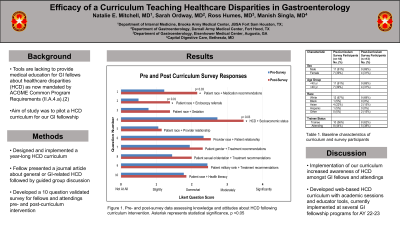
Results: 11 fellows and 7 attendings completed the survey before, and 8 trainees and 5 attendings completed the survey following completion of the curriculum. We found that awareness and knowledge about health disparities improved through the curriculum. As seen in Figure 1, there were statistically significant differences in recognizing the impact of patient race on medication recommendations (p = 0.03) and referrals for endoscopy (p = 0.01), as well as the effect of socioeconomic status and race on medical outcomes (p = 0.03). We also observed that individuals were open to recognizing and sharing personal bias and engaging in discussions about how to improve our systems to reduce disparities.
Discussion: Our results show that implementation of our curriculum increased awareness of healthcare disparities amongst gastroenterology fellows and attendings. Our curriculum is the first of its kind validated through pre- and post-survey results and fulfills an important new ACGME requirement for training programs. This was our first iteration and we have subsequently modified this curriculum to include guided academic sessions and educator tools through an online platform to be implemented at several GI training programs in the US in the 2022-2023 academic year.

Disclosures:
Natalie Mitchell, MD1, Sarah Ordway, MD2, Ross Humes, MD3, Manish Singla, MD4. D0619 - Efficacy of a Curriculum Teaching Healthcare Disparities in Gastroenterology Fellowship, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Brooke Army Medical Center, San Antonio, TX; 2Carl R. Darnall Army Medical Center, Fort Hood, TX; 3Dwight D. Eisenhower Army Medical Center, Fort Gordon, GA; 4Capital Digestive Care, Chevy Chase, MD
Introduction: There are many studies identifying healthcare disparities based on sex, race, and economic status in gastroenterology (GI) influenced by the social determinants of health. The Accreditation Council for Graduate Medical Education (ACGME) recently mandated that medical training programs provide education about healthcare disparities. Tools to provide this education are lacking, and methods to address health equity remain unfamiliar to many health care systems, their leaders, and medical educators. The aim of this study was to pilot a healthcare disparities curriculum for our GI fellowship program.
Methods: Using the Kern 6-step method, we designed a year-long health disparities curriculum and implemented it in our GI fellowship from 2020-2021. During weekly academics, a fellow presented a journal article identifying a disparity in GI followed by guided group discussion about how to apply that study to our own practice and patient population. We developed a validated survey to assess knowledge and attitudes about healthcare disparities before and after implementation of the curriculum.
Results: 11 fellows and 7 attendings completed the survey before, and 8 trainees and 5 attendings completed the survey following completion of the curriculum. We found that awareness and knowledge about health disparities improved through the curriculum. As seen in Figure 1, there were statistically significant differences in recognizing the impact of patient race on medication recommendations (p = 0.03) and referrals for endoscopy (p = 0.01), as well as the effect of socioeconomic status and race on medical outcomes (p = 0.03). We also observed that individuals were open to recognizing and sharing personal bias and engaging in discussions about how to improve our systems to reduce disparities.
Discussion: Our results show that implementation of our curriculum increased awareness of healthcare disparities amongst gastroenterology fellows and attendings. Our curriculum is the first of its kind validated through pre- and post-survey results and fulfills an important new ACGME requirement for training programs. This was our first iteration and we have subsequently modified this curriculum to include guided academic sessions and educator tools through an online platform to be implemented at several GI training programs in the US in the 2022-2023 academic year.

Figure: Figure 1. Pre- and Post-Survey Response Data. Pre-survey data appears in blue. Post-survey data appears in red. Asterisk represents statistically significant questions, p <0.05. Graph demonstrates an overall improvement in awareness about existing healthcare disparities following the implementation of our curriculum.
Disclosures:
Natalie Mitchell indicated no relevant financial relationships.
Sarah Ordway indicated no relevant financial relationships.
Ross Humes indicated no relevant financial relationships.
Manish Singla indicated no relevant financial relationships.
Natalie Mitchell, MD1, Sarah Ordway, MD2, Ross Humes, MD3, Manish Singla, MD4. D0619 - Efficacy of a Curriculum Teaching Healthcare Disparities in Gastroenterology Fellowship, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
