Back

Poster Session A - Sunday Afternoon
Category: Stomach
A0723 - Two Tales of Gastric Mucormycosis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Anurag Sachan, MBBS, MD
Post Graduate Institute of Medical Education and Research
S.A.S. Nagar, Punjab, India
Presenting Author(s)
Anurag Sachan, MBBS, MD1, Arup Choudhury, MBBS2, Arpit Sasani, MBBS, MD2, Harshal Mandavdhare, MBBS, MD, DM2
1Post Graduate Institute of Medical Education and Research, S.A.S. Nagar, Punjab, India; 2Post Graduate Institute of Medical Education and Research, Chandigarh, Chandigarh, India
Introduction: Gastric mucormycosis is a rare but potentially lethal infection seen more often in immunocompromised individuals. Mucormycosis mostly involves upper respiratory tract, orbit, brain or lungs and rarely involves the gastrointestinal (GI) tract. Stomach is the commonest GI site.
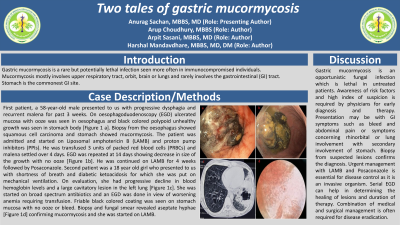
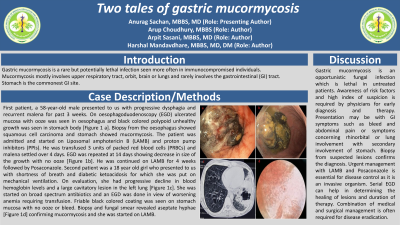
Case Description/Methods: First patient, a 58-year-old male presented to us with progressive dysphagia and recurrent malena for past 3 weeks. On oesophagoduodenoscopy (EGD) ulcerated mucosa with ooze was seen in oesophagus and black colored polypoid unhealthy growth was seen in stomach body [Figure 1 a]. Biopsy from the oesophagus showed squamous cell carcinoma and stomach showed mucormycosis. The patient was admitted and started on Liposomal amphotericin B (LAMB) and proton pump inhibitors(PPIs). He was transfused 3 units of packed red blood cells(PRBCs) and malena settled over 4 days. EGD was repeated at 14 days showing decrease in size of the growth with no ooze [Figure 1b]. He was continued on LAMB for 4 weeks followed by posaconazole.
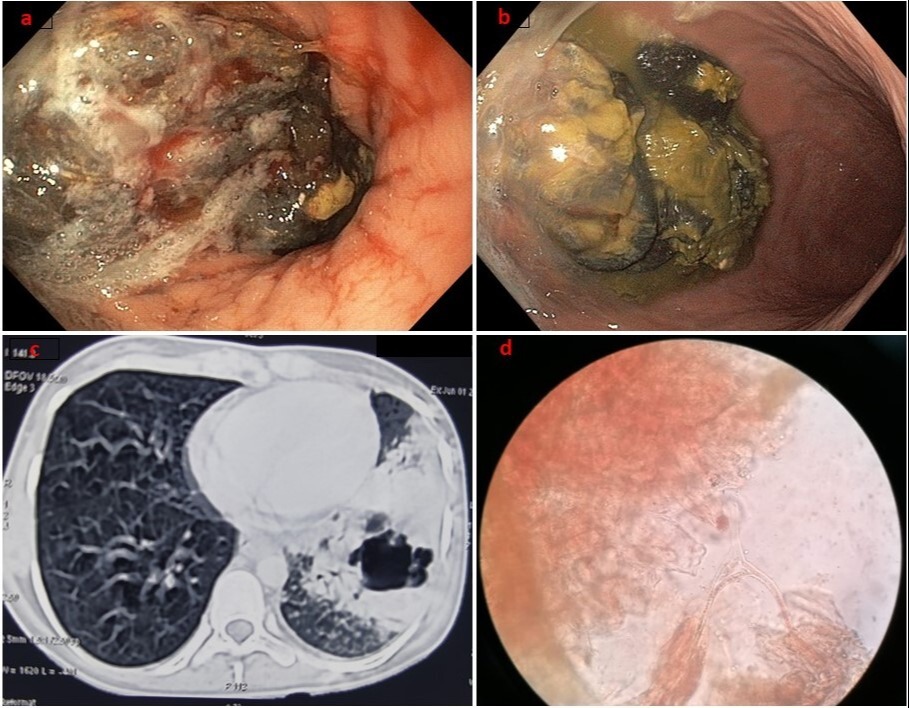
Second patient was a 18 year old girl who presented to us with shortness of breath and diabetic ketoacidosis for which she was put on mechanical ventilation. On evaluation, she had progressive decline in blood hemoglobin levels and a large cavitatory lesion in the left lung [Figure 1c]. She was started on broad spectrum antibiotics and an EGD was done in view of worsening anemia requiring transfusion. Friable black colored coating was seen on stomach mucosa with no ooze or bleed. Biopsy and fungal smear revealed aseptate hyphae [Figure 1d] confirming mucormycosis and she was started on LAMB.
Discussion: Gastric mucormycosis is an opportunistic fungal infection which is lethal in untreated patients. Awareness of risk factors and high index of suspicion is required by physicians for early diagnosis and therapy. Presentation may be with GI symptoms such as bleed and abdominal pain or symptoms concerning rhinorbital or lung involvement with secondary involvement of stomach. Biopsy from suspected lesions confirms the diagnosis. Urgent management with LAMB and Posaconazole is essential for disease control as it is an invasive organism. Serial EGD can help in determining the healing of lesions and duration of therapy. Combination of medical and surgical management is often required for disease eradication.
Disclosures:
Anurag Sachan, MBBS, MD1, Arup Choudhury, MBBS2, Arpit Sasani, MBBS, MD2, Harshal Mandavdhare, MBBS, MD, DM2. A0723 - Two Tales of Gastric Mucormycosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Post Graduate Institute of Medical Education and Research, S.A.S. Nagar, Punjab, India; 2Post Graduate Institute of Medical Education and Research, Chandigarh, Chandigarh, India
Introduction: Gastric mucormycosis is a rare but potentially lethal infection seen more often in immunocompromised individuals. Mucormycosis mostly involves upper respiratory tract, orbit, brain or lungs and rarely involves the gastrointestinal (GI) tract. Stomach is the commonest GI site.
Case Description/Methods: First patient, a 58-year-old male presented to us with progressive dysphagia and recurrent malena for past 3 weeks. On oesophagoduodenoscopy (EGD) ulcerated mucosa with ooze was seen in oesophagus and black colored polypoid unhealthy growth was seen in stomach body [Figure 1 a]. Biopsy from the oesophagus showed squamous cell carcinoma and stomach showed mucormycosis. The patient was admitted and started on Liposomal amphotericin B (LAMB) and proton pump inhibitors(PPIs). He was transfused 3 units of packed red blood cells(PRBCs) and malena settled over 4 days. EGD was repeated at 14 days showing decrease in size of the growth with no ooze [Figure 1b]. He was continued on LAMB for 4 weeks followed by posaconazole.
Second patient was a 18 year old girl who presented to us with shortness of breath and diabetic ketoacidosis for which she was put on mechanical ventilation. On evaluation, she had progressive decline in blood hemoglobin levels and a large cavitatory lesion in the left lung [Figure 1c]. She was started on broad spectrum antibiotics and an EGD was done in view of worsening anemia requiring transfusion. Friable black colored coating was seen on stomach mucosa with no ooze or bleed. Biopsy and fungal smear revealed aseptate hyphae [Figure 1d] confirming mucormycosis and she was started on LAMB.
Discussion: Gastric mucormycosis is an opportunistic fungal infection which is lethal in untreated patients. Awareness of risk factors and high index of suspicion is required by physicians for early diagnosis and therapy. Presentation may be with GI symptoms such as bleed and abdominal pain or symptoms concerning rhinorbital or lung involvement with secondary involvement of stomach. Biopsy from suspected lesions confirms the diagnosis. Urgent management with LAMB and Posaconazole is essential for disease control as it is an invasive organism. Serial EGD can help in determining the healing of lesions and duration of therapy. Combination of medical and surgical management is often required for disease eradication.
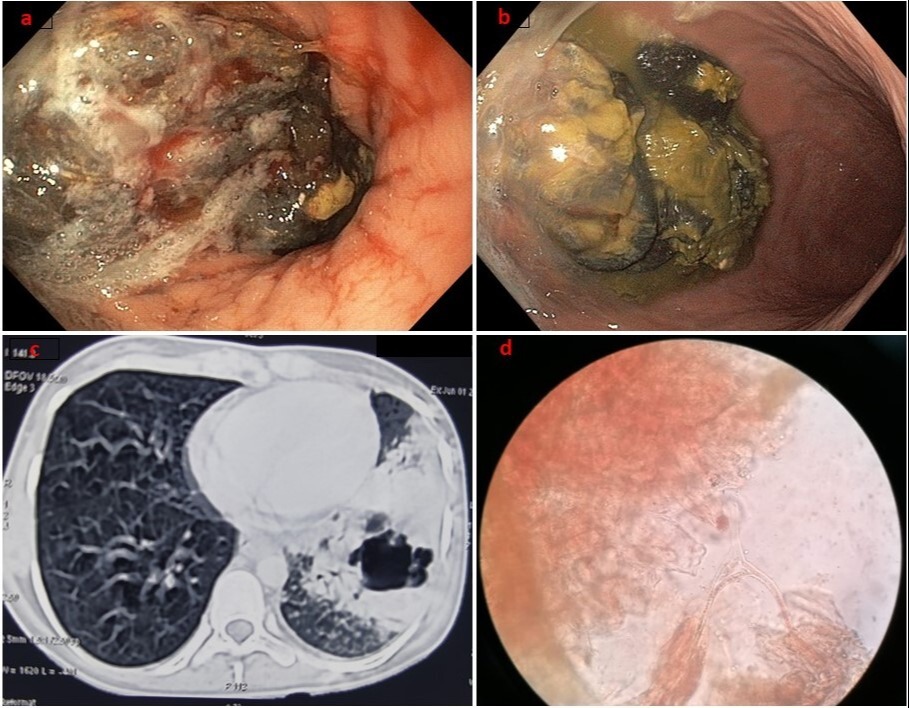
Figure: Figure 1: (a) Black polypoid lesion with ooze (b) Decrease in size and ooze (c) Left cavitary lesion with consolidation (d) Aseptate hyphae seen on smear
Disclosures:
Anurag Sachan indicated no relevant financial relationships.
Arup Choudhury indicated no relevant financial relationships.
Arpit Sasani indicated no relevant financial relationships.
Harshal Mandavdhare indicated no relevant financial relationships.
Anurag Sachan, MBBS, MD1, Arup Choudhury, MBBS2, Arpit Sasani, MBBS, MD2, Harshal Mandavdhare, MBBS, MD, DM2. A0723 - Two Tales of Gastric Mucormycosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
