Back


Poster Session C - Monday Afternoon
Category: Esophagus
C0242 - Achalasia as a Sequelae of COVID-19
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Mohammad Jamil, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Award: Presidential Poster Award
Mohammad Jamil, MD1, Maham Hayat, MD1, Ijlal Akbar Ali, MD1, Bibi Maryam, MD2
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2Bolan Medical College, Oklahoma City, OK
Introduction: Achalasia is a neurodegenerative motility disorder of distal esophagus and lower esophageal sphincter characterized by loss of myenteric neurons in esophagus. It therefore results in deranged peristalsis and characteristic manifestations of regurgitation, dysphagia and retrosternal chest pressure sensation. Recent studies have suggested inflammatory neurodegenerative insult from viral infection as a potential etiology. Sars-Cov-2 causes multiple gastrointestinal (GI) manifestations like ageusia, nausea, vomiting, pain and diarrhea. We present a rare case of achalasia that presented soon after COVID infection in an otherwise healthy male.
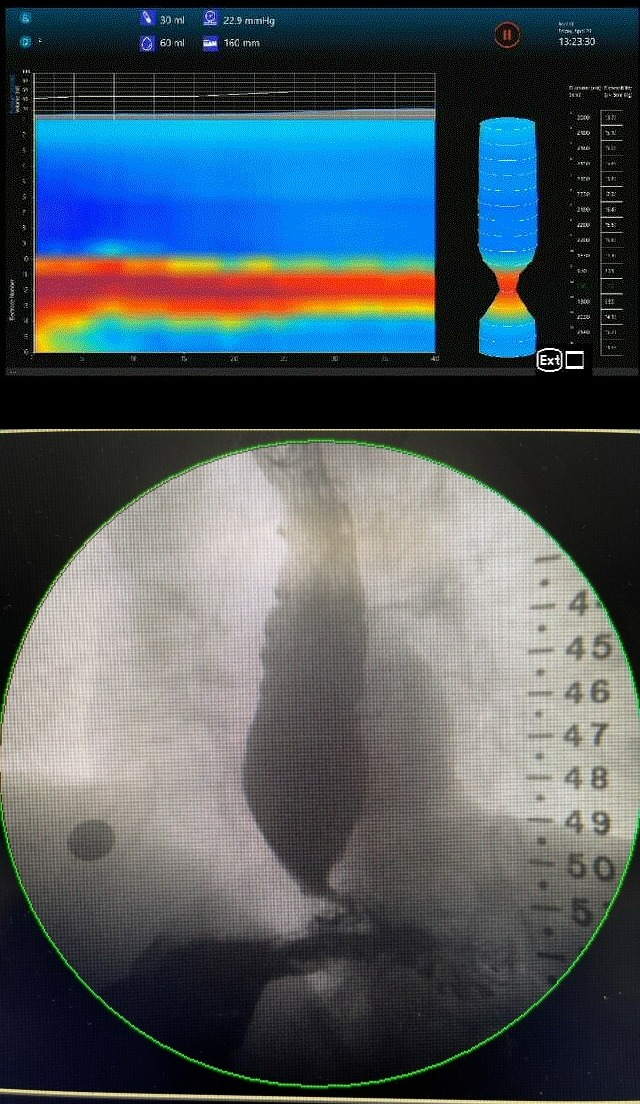
Case Description/Methods: A 63 year old man was referred for further evaluation of dysphagia that started a few months after a non-severe COVID infection with associated ageusia. He reported progressive dysphagia to both solids and liquids with concomitant regurgitation and chest pain. By the time he presented, he had lost 45 lbs over the course of 6 months and had an Eckardt score of 8. High resolution manometry was suggestive of evolving type II achalasia. A follow up Endoflip exam with a 16 cm catheter inflated to 60 cc revealed a esophagogastric diameter of 7.3 mm and a distensibility index (DI) of 1.9. Timed barium esophagogram showed a 5 cm contrast column in distal esophagus at 5 minutes. The patient has since been referred for per oral endoscopic myotomy.
Discussion: Sars-Cov-2 enters the GI epithelial cells through ACE2 receptors and exerts its effects through an aberrant immune response involving T- lymphocytes rather than direct epithelial damage. An anomalous immune reaction resulting in degeneration of inhibitory neurons in the myenteric plexus may be the cause of achalasia in COVID-19. On literature review, we came across at least 1 case report of a patient developing achalasia after COVID-19. A Venezuelan study noted that the frequency of patients with achalasia during the year 2020 and 2021 was far greater than those of previous years and at least 2/3rd of these patients had presented with COVID-19 infection. It will be interesting to note if coronavirus can be isolated from muscle biopsies of these subjects as has been the case with VZV previously. Further investigation especially into patients presenting with GI symptoms with COVID infection is warranted.
Disclosures:
Mohammad Jamil, MD1, Maham Hayat, MD1, Ijlal Akbar Ali, MD1, Bibi Maryam, MD2. C0242 - Achalasia as a Sequelae of COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Mohammad Jamil, MD1, Maham Hayat, MD1, Ijlal Akbar Ali, MD1, Bibi Maryam, MD2
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2Bolan Medical College, Oklahoma City, OK
Introduction: Achalasia is a neurodegenerative motility disorder of distal esophagus and lower esophageal sphincter characterized by loss of myenteric neurons in esophagus. It therefore results in deranged peristalsis and characteristic manifestations of regurgitation, dysphagia and retrosternal chest pressure sensation. Recent studies have suggested inflammatory neurodegenerative insult from viral infection as a potential etiology. Sars-Cov-2 causes multiple gastrointestinal (GI) manifestations like ageusia, nausea, vomiting, pain and diarrhea. We present a rare case of achalasia that presented soon after COVID infection in an otherwise healthy male.
Case Description/Methods: A 63 year old man was referred for further evaluation of dysphagia that started a few months after a non-severe COVID infection with associated ageusia. He reported progressive dysphagia to both solids and liquids with concomitant regurgitation and chest pain. By the time he presented, he had lost 45 lbs over the course of 6 months and had an Eckardt score of 8. High resolution manometry was suggestive of evolving type II achalasia. A follow up Endoflip exam with a 16 cm catheter inflated to 60 cc revealed a esophagogastric diameter of 7.3 mm and a distensibility index (DI) of 1.9. Timed barium esophagogram showed a 5 cm contrast column in distal esophagus at 5 minutes. The patient has since been referred for per oral endoscopic myotomy.
Discussion: Sars-Cov-2 enters the GI epithelial cells through ACE2 receptors and exerts its effects through an aberrant immune response involving T- lymphocytes rather than direct epithelial damage. An anomalous immune reaction resulting in degeneration of inhibitory neurons in the myenteric plexus may be the cause of achalasia in COVID-19. On literature review, we came across at least 1 case report of a patient developing achalasia after COVID-19. A Venezuelan study noted that the frequency of patients with achalasia during the year 2020 and 2021 was far greater than those of previous years and at least 2/3rd of these patients had presented with COVID-19 infection. It will be interesting to note if coronavirus can be isolated from muscle biopsies of these subjects as has been the case with VZV previously. Further investigation especially into patients presenting with GI symptoms with COVID infection is warranted.
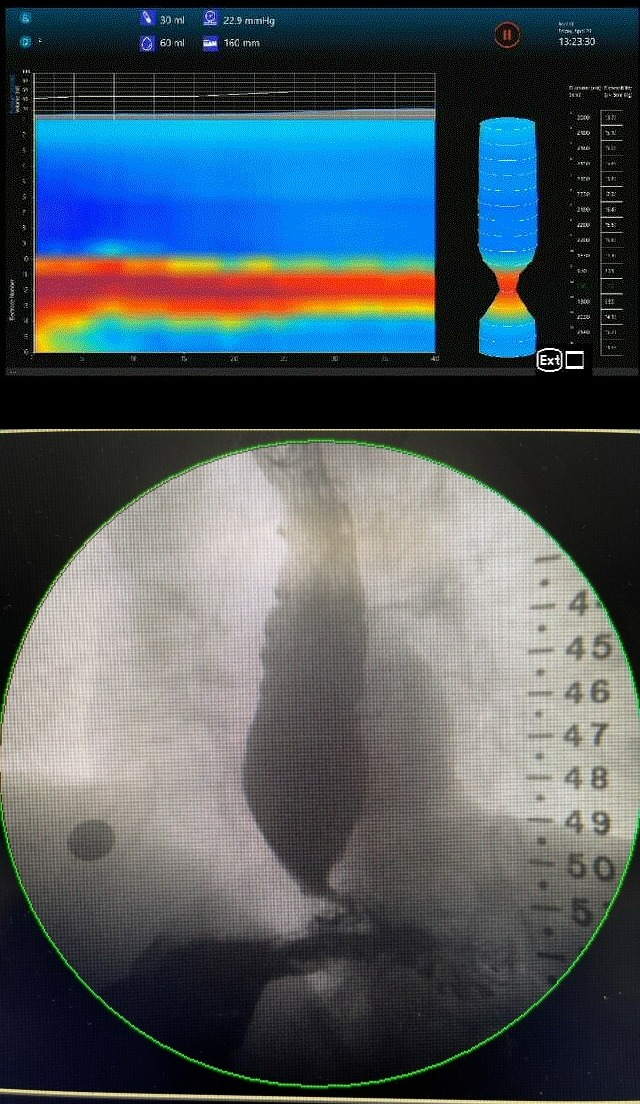
Figure: Endoflip ; Barium Esophageogram
Disclosures:
Mohammad Jamil indicated no relevant financial relationships.
Maham Hayat indicated no relevant financial relationships.
Ijlal Akbar Ali indicated no relevant financial relationships.
Bibi Maryam indicated no relevant financial relationships.
Mohammad Jamil, MD1, Maham Hayat, MD1, Ijlal Akbar Ali, MD1, Bibi Maryam, MD2. C0242 - Achalasia as a Sequelae of COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

