Back

Poster Session B - Monday Morning
Category: Colon
B0157 - Chronic Lymphocytic Leukemia Presenting as Colonic Ulcers
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Melanie Burgos, MD
CarePoint Health
Bayonne, NJ
Presenting Author(s)
Melanie Burgos, MD1, Nha Duong, DO1, Joseph Constantino, DO1, David Gay, MD2, Benjamin Kuritzkes, MD3, Jennifer Hsieh, MD1, Jonelle George, DO1
1CarePoint Health, Bayonne, NJ; 2CarePoint Health, Jersey City, NJ; 3Columbia University, New York, NY
Introduction: Chronic Lymphocytic Leukemia (CLL) accounts for 25% of leukemias. One can present with hepatomegaly, splenomegaly, and lymphadenopathy. CLL infiltration in the gastrointestinal (GI) mucosa is rare. Colonic CLL can develop late in the disease course with mild to no GI symptoms. Awareness of CLL and its various extra-nodal presentations allow for prompt diagnosis and treatment.
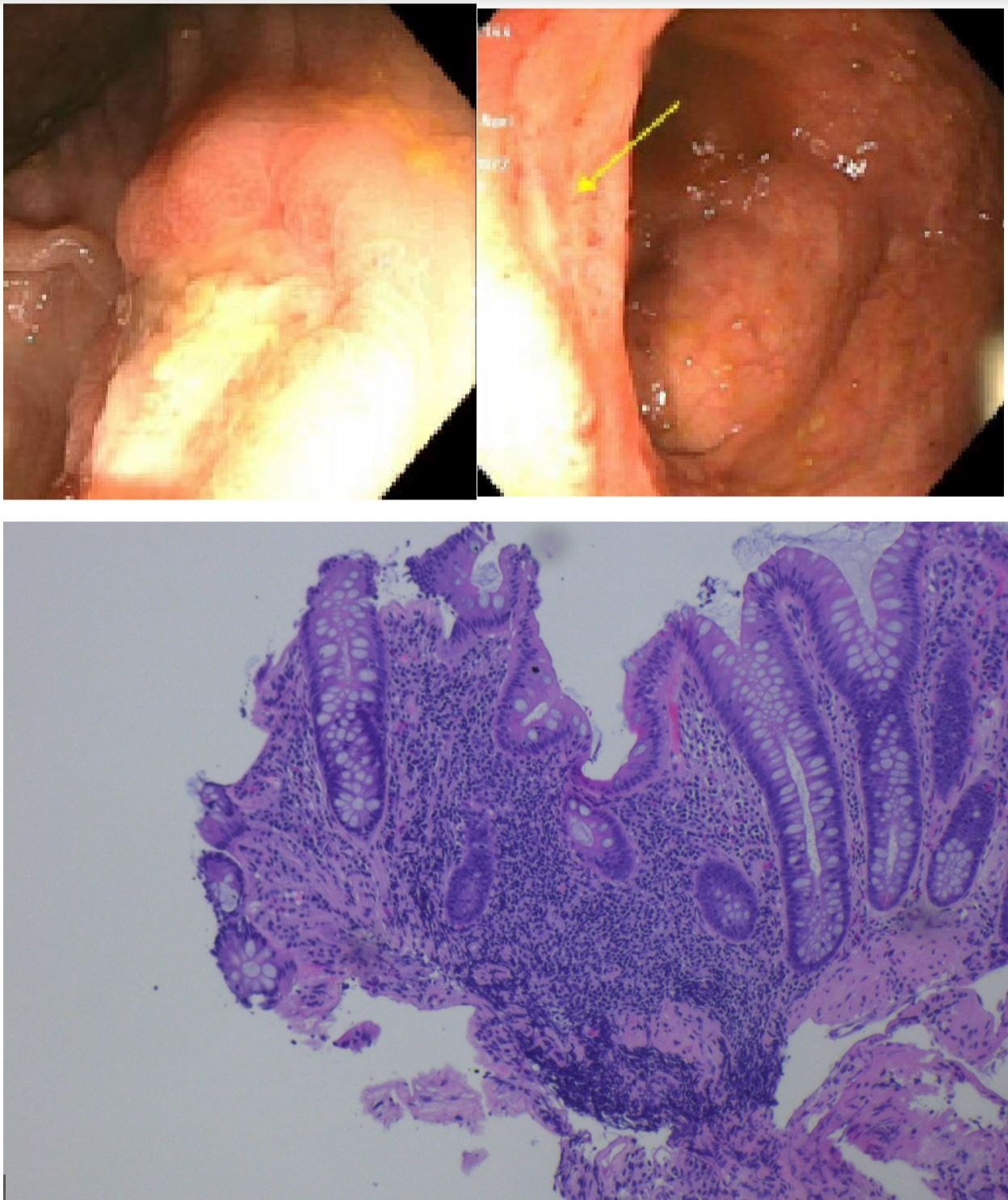
Case Description/Methods: An 80-year-old female with untreated CLL presented with two months of rectal bleeding. She denied weight loss, anorexia, night sweats, blood thinners, and NSAID use. She had WBC 34.3, platelets 139, and a normal Hgb of 13.2. Colonoscopy showed ulcerations at the ileocecal valve and transverse colon, a 30 mm ascending colon polyp, and multiple 10-20 mm transverse and descending colon polyps. Pathology showed only chronic inflammation of the ulcerated regions, and a sessile serrated adenoma at the ascending colon. The remaining polyps were not removed due to concern for cancer and potential colectomy. A CT chest, abdomen, and pelvis was unremarkable. Tumor markers showed CEA 8 and normal Ca19-9 and Ca-125. Due to an unclear diagnosis, a second colonoscopy was performed with repeat biopsies and removal of all polyps in the descending and sigmoid colon. Pathology results were negative for inflammatory bowel disease and infection. The polyps were tubular adenomas and hyperplastic. However, immunohistochemical analysis was positive for CD5/CD43 and CD23, indicative of CLL in the ulcerated mucosa. Treatment options were discussed with surgery and oncology. The patient was offered right colon resection or endoscopic removal of the remaining polyps prior to chemotherapy.
Discussion: Colorectal lymphomas are rare and account for 1% of all GI malignancies with CLL usually found proximal to the hepatic flexure. In this case, the presence of ulcerations and large polyps were concerning for colorectal cancer. However, the initial work-up was negative. After a repeat colonoscopy, testing for specific CLL markers was requested. In a review of literature, chemotherapy alone for colonic CLL had a perforation risk of 15%. While it is unclear if surgical treatment is beneficial, it is a potential option. Due to the high risk of perforation on chemotherapy, recommendations included right hemicolectomy or endoscopic removal of the remaining polyps prior to starting treatment. This demonstrates the importance of knowing the varying presentations of colonic CLL as its treatment may require multidisciplinary discussion.
Disclosures:
Melanie Burgos, MD1, Nha Duong, DO1, Joseph Constantino, DO1, David Gay, MD2, Benjamin Kuritzkes, MD3, Jennifer Hsieh, MD1, Jonelle George, DO1. B0157 - Chronic Lymphocytic Leukemia Presenting as Colonic Ulcers, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1CarePoint Health, Bayonne, NJ; 2CarePoint Health, Jersey City, NJ; 3Columbia University, New York, NY
Introduction: Chronic Lymphocytic Leukemia (CLL) accounts for 25% of leukemias. One can present with hepatomegaly, splenomegaly, and lymphadenopathy. CLL infiltration in the gastrointestinal (GI) mucosa is rare. Colonic CLL can develop late in the disease course with mild to no GI symptoms. Awareness of CLL and its various extra-nodal presentations allow for prompt diagnosis and treatment.
Case Description/Methods: An 80-year-old female with untreated CLL presented with two months of rectal bleeding. She denied weight loss, anorexia, night sweats, blood thinners, and NSAID use. She had WBC 34.3, platelets 139, and a normal Hgb of 13.2. Colonoscopy showed ulcerations at the ileocecal valve and transverse colon, a 30 mm ascending colon polyp, and multiple 10-20 mm transverse and descending colon polyps. Pathology showed only chronic inflammation of the ulcerated regions, and a sessile serrated adenoma at the ascending colon. The remaining polyps were not removed due to concern for cancer and potential colectomy. A CT chest, abdomen, and pelvis was unremarkable. Tumor markers showed CEA 8 and normal Ca19-9 and Ca-125. Due to an unclear diagnosis, a second colonoscopy was performed with repeat biopsies and removal of all polyps in the descending and sigmoid colon. Pathology results were negative for inflammatory bowel disease and infection. The polyps were tubular adenomas and hyperplastic. However, immunohistochemical analysis was positive for CD5/CD43 and CD23, indicative of CLL in the ulcerated mucosa. Treatment options were discussed with surgery and oncology. The patient was offered right colon resection or endoscopic removal of the remaining polyps prior to chemotherapy.
Discussion: Colorectal lymphomas are rare and account for 1% of all GI malignancies with CLL usually found proximal to the hepatic flexure. In this case, the presence of ulcerations and large polyps were concerning for colorectal cancer. However, the initial work-up was negative. After a repeat colonoscopy, testing for specific CLL markers was requested. In a review of literature, chemotherapy alone for colonic CLL had a perforation risk of 15%. While it is unclear if surgical treatment is beneficial, it is a potential option. Due to the high risk of perforation on chemotherapy, recommendations included right hemicolectomy or endoscopic removal of the remaining polyps prior to starting treatment. This demonstrates the importance of knowing the varying presentations of colonic CLL as its treatment may require multidisciplinary discussion.
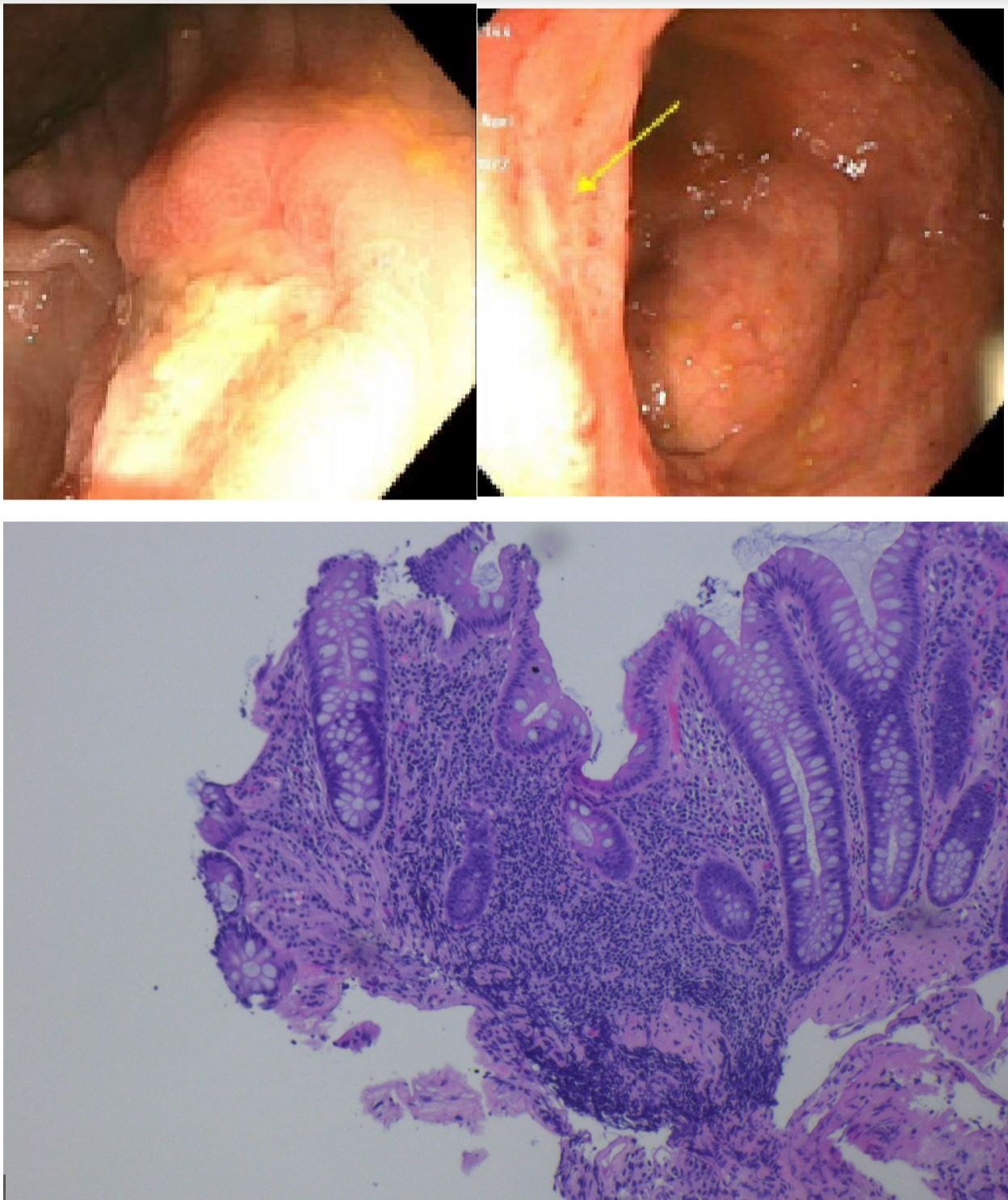
Figure: Colonic ulcers located at the transverse colon (top left) and IC valve (top right). H&E stain of the colonic mucosa (bottom) that showed positive markers for CLL on IHC analysis.
Disclosures:
Melanie Burgos indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Joseph Constantino indicated no relevant financial relationships.
David Gay indicated no relevant financial relationships.
Benjamin Kuritzkes indicated no relevant financial relationships.
Jennifer Hsieh indicated no relevant financial relationships.
Jonelle George indicated no relevant financial relationships.
Melanie Burgos, MD1, Nha Duong, DO1, Joseph Constantino, DO1, David Gay, MD2, Benjamin Kuritzkes, MD3, Jennifer Hsieh, MD1, Jonelle George, DO1. B0157 - Chronic Lymphocytic Leukemia Presenting as Colonic Ulcers, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
