Back

Poster Session C - Monday Afternoon
Category: Esophagus
C0230 - The Esophagus and Beyond: A Case of Refractory Chest Pain
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- NS
Noor Siddiqi Syed, MD
Santa Clara Valley Medical Center
Saratoga, CA
Presenting Author(s)
Noor S. Syed, MD1, Linda Nguyen, MD2
1Santa Clara Valley Medical Center, Saratoga, CA; 2Stanford University School of Medicine, Redwood City, CA
Introduction: Esophageal disorders are a common etiology for noncardiac chest pain, including esophagogastric junction outlet obstruction(EGJOO). Herein, we describe a case of a patient with EGJOO with refractory chest pain who was ultimately found to have Hereditary alpha-tryptasemia(HaT). This rare presentation allows clinicians to broaden the differential when investigating noncardiac chest pain.
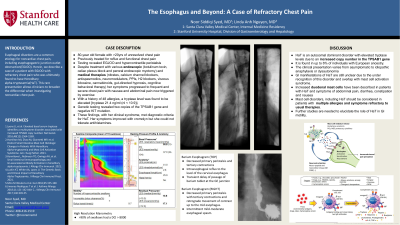
Case Description/Methods: The case is an 80-year old female with two decades of unresolved chest pain. For years, she was treated for reflux and functional chest pain. Subsequent testing revealed EGJOO and hypercontractile peristalsis. Despite treatment with various endoscopic (botulinum toxin, celiac plexus block and peroral endoscopic myotomy) and medical therapies (nitrates, calcium channel blockers, antispasmodics, neuromodulators, PPIs, H2 blockers, viscous lidocaine, cannabinoids, gut-directed hypnosis, cognitive behavioral therapy) her symptoms progressed to frequent and severe chest pain with nausea and abdominal pain. She became intolerant to all foods with symptoms now triggered by exercise. With a history of 48 allergies, a tryptase level was found to be elevated [tryptase 21.4 ng/ml (nl < 10.9)]. Genetic testing revealed two copies of the TPSAB1 gene and negative KIT mutation. These findings, with her clinical syndrome, met diagnostic criteria for HaT[1,2]. Her symptoms improved with cromolyn but she could not tolerate antihistamines.
Discussion: HaT is an autosomal dominant disorder with elevated tryptase levels due to an increased copy number in the TPSAB1 gene[1]. It is found in up to 6% of individuals with European ancestry. The clinical presentation varies ranging from asymptomatic to idiopathic anaphylaxis or dysautonomia[1]. GI manifestations of HaT are still unclear due to the under recognition of this disorder and overlap with mast cell activation syndrome. Increased duodenal mast cells have been described in patients with HaT and symptoms of abdominal pain, diarrhea, constipation and nausea[2]. The objective of this case is to bring awareness of HaT to the GI community to promote early diagnosis, especially in patients presenting with multiple allergies and refractory symptoms. Further studies are needed to elucidate the role of HaT in GI motility.
Disclosures:
Noor S. Syed, MD1, Linda Nguyen, MD2. C0230 - The Esophagus and Beyond: A Case of Refractory Chest Pain, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Santa Clara Valley Medical Center, Saratoga, CA; 2Stanford University School of Medicine, Redwood City, CA
Introduction: Esophageal disorders are a common etiology for noncardiac chest pain, including esophagogastric junction outlet obstruction(EGJOO). Herein, we describe a case of a patient with EGJOO with refractory chest pain who was ultimately found to have Hereditary alpha-tryptasemia(HaT). This rare presentation allows clinicians to broaden the differential when investigating noncardiac chest pain.
Case Description/Methods: The case is an 80-year old female with two decades of unresolved chest pain. For years, she was treated for reflux and functional chest pain. Subsequent testing revealed EGJOO and hypercontractile peristalsis. Despite treatment with various endoscopic (botulinum toxin, celiac plexus block and peroral endoscopic myotomy) and medical therapies (nitrates, calcium channel blockers, antispasmodics, neuromodulators, PPIs, H2 blockers, viscous lidocaine, cannabinoids, gut-directed hypnosis, cognitive behavioral therapy) her symptoms progressed to frequent and severe chest pain with nausea and abdominal pain. She became intolerant to all foods with symptoms now triggered by exercise. With a history of 48 allergies, a tryptase level was found to be elevated [tryptase 21.4 ng/ml (nl < 10.9)]. Genetic testing revealed two copies of the TPSAB1 gene and negative KIT mutation. These findings, with her clinical syndrome, met diagnostic criteria for HaT[1,2]. Her symptoms improved with cromolyn but she could not tolerate antihistamines.
Discussion: HaT is an autosomal dominant disorder with elevated tryptase levels due to an increased copy number in the TPSAB1 gene[1]. It is found in up to 6% of individuals with European ancestry. The clinical presentation varies ranging from asymptomatic to idiopathic anaphylaxis or dysautonomia[1]. GI manifestations of HaT are still unclear due to the under recognition of this disorder and overlap with mast cell activation syndrome. Increased duodenal mast cells have been described in patients with HaT and symptoms of abdominal pain, diarrhea, constipation and nausea[2]. The objective of this case is to bring awareness of HaT to the GI community to promote early diagnosis, especially in patients presenting with multiple allergies and refractory symptoms. Further studies are needed to elucidate the role of HaT in GI motility.
- Lyons, et al. Elevated basal serum tryptase identifies a multisystem disorder associated with increased TPSAB1 copy number. 2016;1564.
- Hamilton, et al. Distinct Small Intestine Mast Cell Histologic Changes in Patients With HaT and MCAS. 2021: 997.
Disclosures:
Noor Syed indicated no relevant financial relationships.
Linda Nguyen indicated no relevant financial relationships.
Noor S. Syed, MD1, Linda Nguyen, MD2. C0230 - The Esophagus and Beyond: A Case of Refractory Chest Pain, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
