Back

Poster Session D - Tuesday Morning
Category: Small Intestine
D0656 - ANCA-Associated Leukocytoclastic Vasculitis With Mesenteric Involvement
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Yan Chu, MD
Saint Louis University School of Medicine
St. Louis, MO
Presenting Author(s)
Yan Chu, MD1, Michelle Baliss, DO2, Michael Presti, MD3, Gregory Sayuk, MD, MPH4, Jill E. Elwing, MD5
1Saint Louis University School of Medicine, St. Louis, MO; 2Saint Louis University, St. Louis, MO; 3St. Louis VA, Saint Louis University, St. Louis, MO; 4St. Louis VA, Washington University School of Medicine, St. Louis, MO; 5St. Louis VA, Washington University, St. Louis, MO
Introduction: Leukocytoclastic vasculitis (LCV) is a usually self-limiting, idiopathic small-vessel vasculitis with cutaneous symptoms. Extracutaneous manifestations should raise suspicion for underlying autoimmune conditions such as ANCA-associated vasculitis, of which LCV may be the initial manifestation. Mesenteric involvement is uncommon and usually represents advanced disease. Delay in recognition of mesenteric vasculitis can lead to progression and perforation. We present a case of gastrointestinal (GI) hemorrhage caused by ANCA-associated LCV.
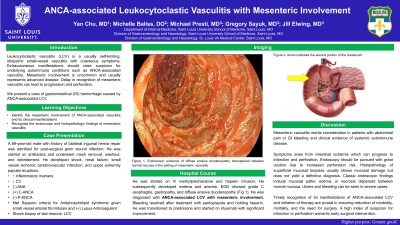
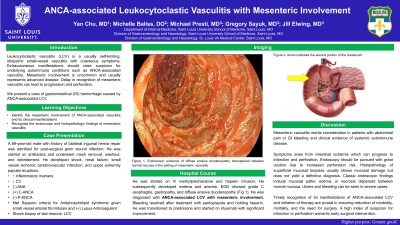
Case Description/Methods: A 69-year-old male with a history of bilateral inguinal hernia repair was admitted for post-surgical groin wound infection. He was started on antibiotics and underwent mesh removal, washout, and debridement. He developed shock, renal failure, small vessel ischemic cerebrovascular infarction, and upper extremity papular eruptions. Work-up was notable for elevated inflammatory markers, decreased C3, negative ANA, positive C-ANCA and negative P-ANCA. He met Sapporo criteria for antiphospholipid syndrome given small vessel arterial thrombosis and positive lupus anticoagulant. Shave biopsy of skin lesions confirmed LCV. He was started on IV methylprednisolone and heparin infusion. He subsequently developed melena and anemia. EGD showed grade C esophagitis, gastropathy, and diffuse erosive duodenopathy (Fig 1). He was diagnosed with ANCA-associated LCV with mesenteric involvement. Bleeding resolved after holding heparin and treatment with pantoprazole. He was transitioned to prednisone and started on rituximab with significant improvement.
Discussion: Though uncommon, mesenteric vasculitis merits consideration in patients with abdominal pain or GI bleeding and clinical evidence of systemic autoimmune disease. Symptoms arise from intestinal ischemia which can progress to infarction and perforation if untreated. Endoscopy should be pursued with great caution due to increased perforation risk. Histopathology of superficial mucosal biopsies usually shows mucosal damage but does not yield a definitive diagnosis. Classic endoscopic findings include mucosal pallor, edema, or necrosis dispersed between normal mucosa. Ulcers and bleeding can be seen in severe cases. Timely recognition of GI manifestations of ANCA-associated LCV and initiation of therapy are pivotal in ensuring reduction of morbidity, mortality, and the need for surgery. A high index of suspicion for infarction or perforation warrants early surgical intervention.

Disclosures:
Yan Chu, MD1, Michelle Baliss, DO2, Michael Presti, MD3, Gregory Sayuk, MD, MPH4, Jill E. Elwing, MD5. D0656 - ANCA-Associated Leukocytoclastic Vasculitis With Mesenteric Involvement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Saint Louis University School of Medicine, St. Louis, MO; 2Saint Louis University, St. Louis, MO; 3St. Louis VA, Saint Louis University, St. Louis, MO; 4St. Louis VA, Washington University School of Medicine, St. Louis, MO; 5St. Louis VA, Washington University, St. Louis, MO
Introduction: Leukocytoclastic vasculitis (LCV) is a usually self-limiting, idiopathic small-vessel vasculitis with cutaneous symptoms. Extracutaneous manifestations should raise suspicion for underlying autoimmune conditions such as ANCA-associated vasculitis, of which LCV may be the initial manifestation. Mesenteric involvement is uncommon and usually represents advanced disease. Delay in recognition of mesenteric vasculitis can lead to progression and perforation. We present a case of gastrointestinal (GI) hemorrhage caused by ANCA-associated LCV.
Case Description/Methods: A 69-year-old male with a history of bilateral inguinal hernia repair was admitted for post-surgical groin wound infection. He was started on antibiotics and underwent mesh removal, washout, and debridement. He developed shock, renal failure, small vessel ischemic cerebrovascular infarction, and upper extremity papular eruptions. Work-up was notable for elevated inflammatory markers, decreased C3, negative ANA, positive C-ANCA and negative P-ANCA. He met Sapporo criteria for antiphospholipid syndrome given small vessel arterial thrombosis and positive lupus anticoagulant. Shave biopsy of skin lesions confirmed LCV. He was started on IV methylprednisolone and heparin infusion. He subsequently developed melena and anemia. EGD showed grade C esophagitis, gastropathy, and diffuse erosive duodenopathy (Fig 1). He was diagnosed with ANCA-associated LCV with mesenteric involvement. Bleeding resolved after holding heparin and treatment with pantoprazole. He was transitioned to prednisone and started on rituximab with significant improvement.
Discussion: Though uncommon, mesenteric vasculitis merits consideration in patients with abdominal pain or GI bleeding and clinical evidence of systemic autoimmune disease. Symptoms arise from intestinal ischemia which can progress to infarction and perforation if untreated. Endoscopy should be pursued with great caution due to increased perforation risk. Histopathology of superficial mucosal biopsies usually shows mucosal damage but does not yield a definitive diagnosis. Classic endoscopic findings include mucosal pallor, edema, or necrosis dispersed between normal mucosa. Ulcers and bleeding can be seen in severe cases. Timely recognition of GI manifestations of ANCA-associated LCV and initiation of therapy are pivotal in ensuring reduction of morbidity, mortality, and the need for surgery. A high index of suspicion for infarction or perforation warrants early surgical intervention.

Figure: Figure 1. Endoscopic evidence of diffuse erosive duodenopathy interspersed between normal mucosa in the setting of mesenteric vasculitis
Disclosures:
Yan Chu indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Michael Presti indicated no relevant financial relationships.
Gregory Sayuk indicated no relevant financial relationships.
Jill Elwing indicated no relevant financial relationships.
Yan Chu, MD1, Michelle Baliss, DO2, Michael Presti, MD3, Gregory Sayuk, MD, MPH4, Jill E. Elwing, MD5. D0656 - ANCA-Associated Leukocytoclastic Vasculitis With Mesenteric Involvement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
