Back

Poster Session D - Tuesday Morning
Category: Small Intestine
D0673 - Sevelamer-Induced Ischemic Ulcerative Colitis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- AB
Aaron Brenner, MD
University of Kentucky College of Medicine
Lexington, KY
Presenting Author(s)
Aaron Brenner, MD1, Cody Kern, MD2, Eun Lee, MD2, Deborah Flomenhoft, MD2
1University of Kentucky College of Medicine, Lexington, KY; 2University of Kentucky, Lexington, KY
Introduction: Sevelamer is phosphate binder used to treat hyperphosphatemia in patients with end stage renal disease (ESRD) on hemodialysis. Rarely, it has been shown to be a cause of ischemic colitis. This case provides an example of a patient presentation and key findings when considering sevelamer induced small bowel ischemic colitis.
Case Description/Methods: A thirty-five-year-old male with ESRD on peritoneal dialysis presented with two days of hematochezia and severe abdominal pain. Diarrhea is described as maroon colored with four episodes in the span of 24 hours. Infectious work-up, including clostridium difficile and comprehensive GI panel, was negative for acute infection. CRP was elevated to 42.6 mg/L, WBC 12.9 10*3/uL, and hemoglobin 7.5 g/dL. CT angiography of the abdomen showed two short segments in the small bowel with inflammation concerning for ischemia.
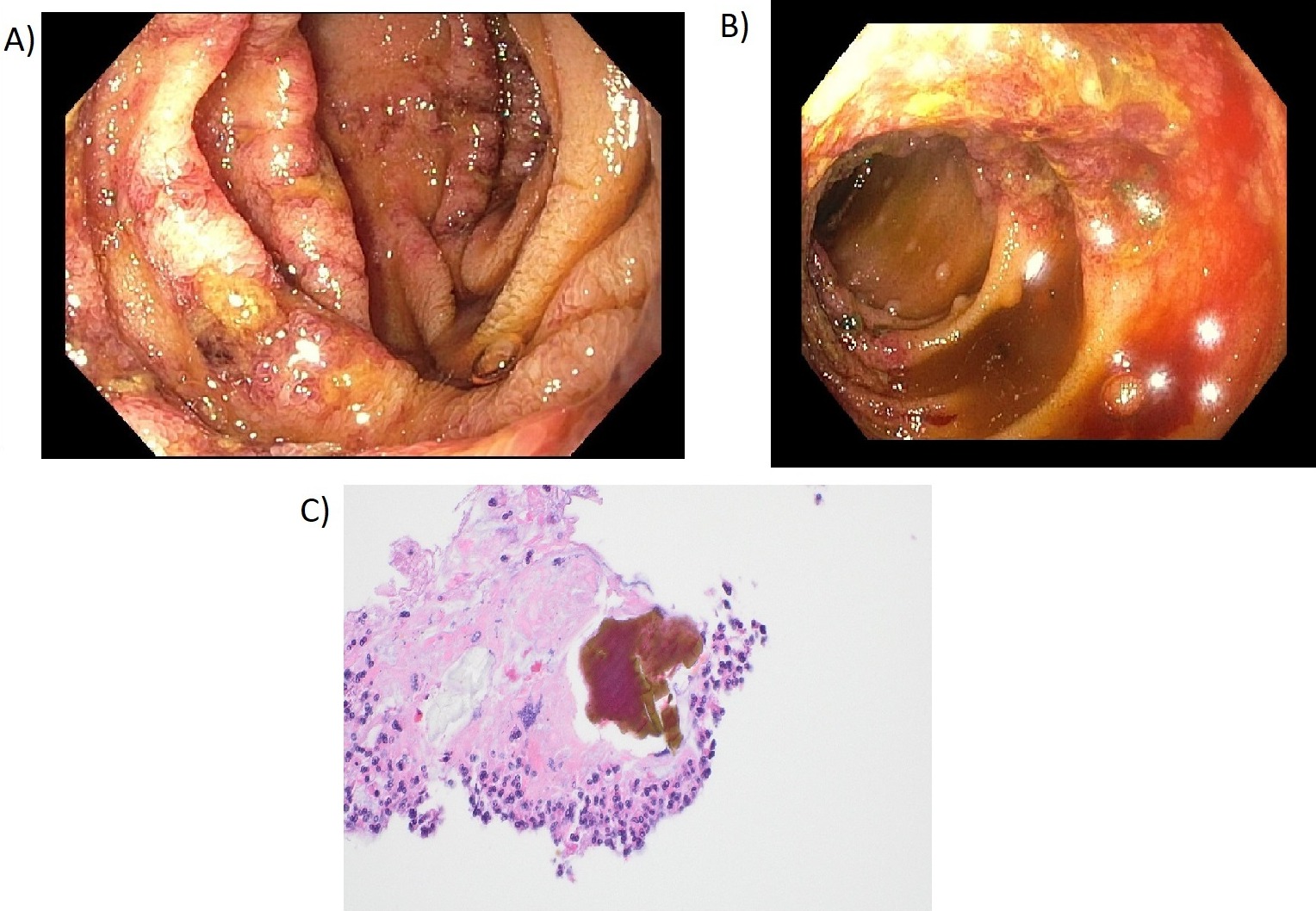
Colonoscopy and push enteroscopy were performed on day three of hospitalization showing ulcerative inflammation in D4 and in the terminal ileum 6cm proximal to the ileocecal valve. Biopsy results at the terminal ileum and D4 were showed mucosal necrosis and acute inflammation with crystalloid structures consistent with pill-associated mucosal necrosis. Further history was obtained from patient, he had been started on sevelamer a few weeks prior to hospitalization. Sevelamer was discontinued resulting in resolution of patient’s symptoms.
Discussion: Although a rare complication, sevelamer has been documented to cause ischemic colitis (Yuste, Keri). These patients present similarly to the one discussed above with melena and abdominal pain. One of the hallmark findings reported on histopathological exam is “fish-scale” crystalloid structures in the mucosa. A review from 2017 examined published case reports in which sevelamer had caused ischemic colitis and the crystalloid structures were present in 13 out of 16 patients (Yuste).
In ESRD patients on sevelamer, who present with symptoms consistent with gastrointestinal bleeding, it is important to recognize the sevelamer as a cause of ischemic colitis and to stop the sevelamer immediately. Furthermore, video capsule endoscopy or push enteroscopy should be considered if standard upper endoscopy and colonoscopy do not identify the source, as sevelamer induced enteritis can occur throughout the intestinal tract. If sevelamer is not stopped, complications such as perforation, acute anemia, stricture formation, and ulceration can continue to occur and worsen.
Disclosures:
Aaron Brenner, MD1, Cody Kern, MD2, Eun Lee, MD2, Deborah Flomenhoft, MD2. D0673 - Sevelamer-Induced Ischemic Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kentucky College of Medicine, Lexington, KY; 2University of Kentucky, Lexington, KY
Introduction: Sevelamer is phosphate binder used to treat hyperphosphatemia in patients with end stage renal disease (ESRD) on hemodialysis. Rarely, it has been shown to be a cause of ischemic colitis. This case provides an example of a patient presentation and key findings when considering sevelamer induced small bowel ischemic colitis.
Case Description/Methods: A thirty-five-year-old male with ESRD on peritoneal dialysis presented with two days of hematochezia and severe abdominal pain. Diarrhea is described as maroon colored with four episodes in the span of 24 hours. Infectious work-up, including clostridium difficile and comprehensive GI panel, was negative for acute infection. CRP was elevated to 42.6 mg/L, WBC 12.9 10*3/uL, and hemoglobin 7.5 g/dL. CT angiography of the abdomen showed two short segments in the small bowel with inflammation concerning for ischemia.
Colonoscopy and push enteroscopy were performed on day three of hospitalization showing ulcerative inflammation in D4 and in the terminal ileum 6cm proximal to the ileocecal valve. Biopsy results at the terminal ileum and D4 were showed mucosal necrosis and acute inflammation with crystalloid structures consistent with pill-associated mucosal necrosis. Further history was obtained from patient, he had been started on sevelamer a few weeks prior to hospitalization. Sevelamer was discontinued resulting in resolution of patient’s symptoms.
Discussion: Although a rare complication, sevelamer has been documented to cause ischemic colitis (Yuste, Keri). These patients present similarly to the one discussed above with melena and abdominal pain. One of the hallmark findings reported on histopathological exam is “fish-scale” crystalloid structures in the mucosa. A review from 2017 examined published case reports in which sevelamer had caused ischemic colitis and the crystalloid structures were present in 13 out of 16 patients (Yuste).
In ESRD patients on sevelamer, who present with symptoms consistent with gastrointestinal bleeding, it is important to recognize the sevelamer as a cause of ischemic colitis and to stop the sevelamer immediately. Furthermore, video capsule endoscopy or push enteroscopy should be considered if standard upper endoscopy and colonoscopy do not identify the source, as sevelamer induced enteritis can occur throughout the intestinal tract. If sevelamer is not stopped, complications such as perforation, acute anemia, stricture formation, and ulceration can continue to occur and worsen.
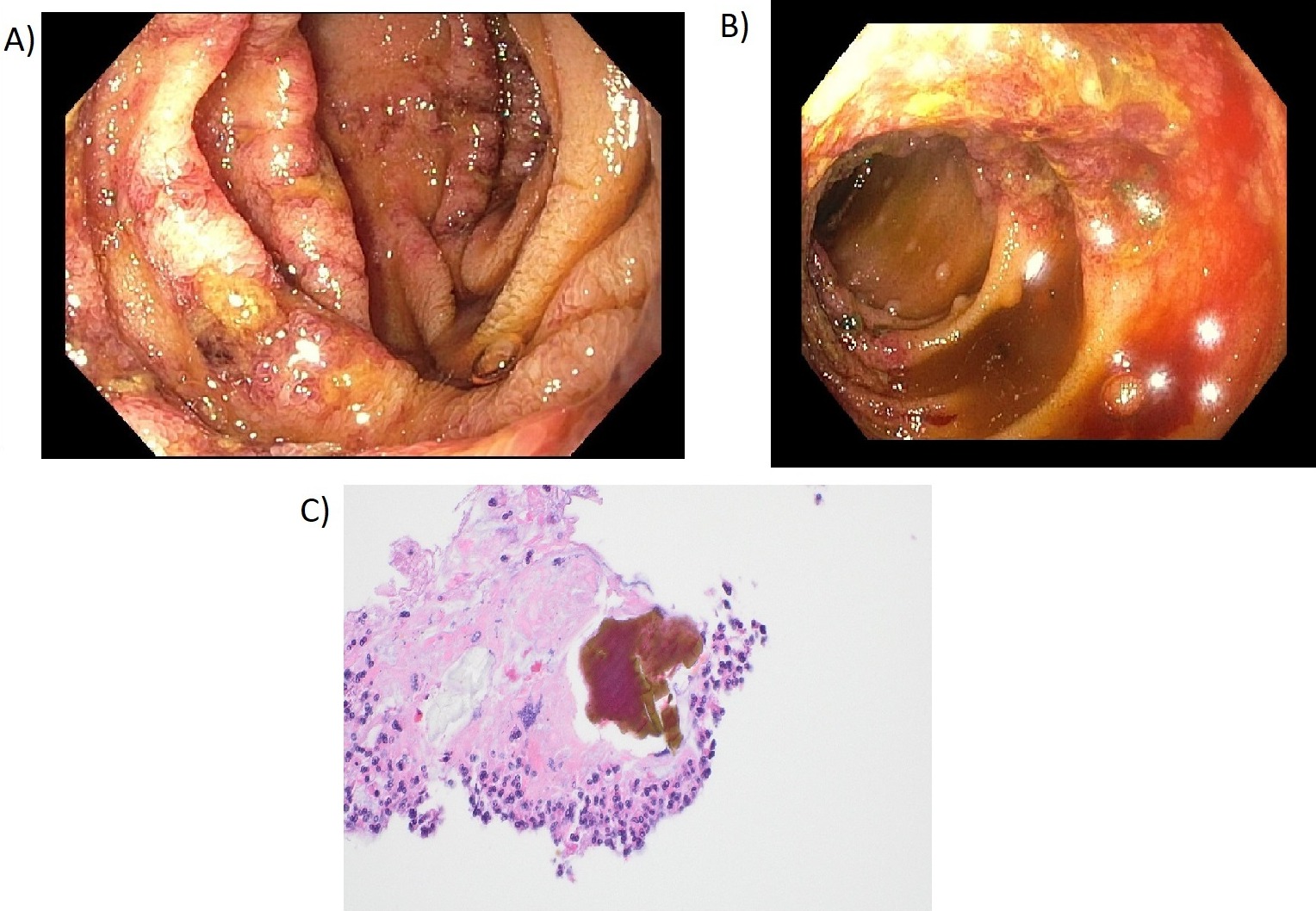
Figure: Figure 1: A) Diffuse ulcerated mucosa of the fourth portion of the duodenum. B) Patchy ulcerations of the terminal ileum. C) Terminal ileum biopsy showing crystalloid structures in an area of necrosis suspicious for pill-associated mucosal necrosis.
Disclosures:
Aaron Brenner indicated no relevant financial relationships.
Cody Kern indicated no relevant financial relationships.
Eun Lee indicated no relevant financial relationships.
Deborah Flomenhoft indicated no relevant financial relationships.
Aaron Brenner, MD1, Cody Kern, MD2, Eun Lee, MD2, Deborah Flomenhoft, MD2. D0673 - Sevelamer-Induced Ischemic Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
