Back

Poster Session B - Monday Morning
Category: Liver
B0622 - A Case of Immediate Hepatitis C Infection Leading to Cholestatic Hepatitis With Significant Viremia After Liver Transplantation
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Parth M. Patel, MD
Henry Ford Jackson
Jackson, MI
Presenting Author(s)
Parth M. Patel, MD1, Hamna Fahad, MD2, Hassan Zreik, MD1, Zarqa Yasin, MD1, Mehak Bhatia, MD1, Syed-Mohammed Jafri, MD2
1Henry Ford Jackson, Jackson, MI; 2Henry Ford Health System, Detroit, MI
Introduction: With the success of direct active antiviral therapy (DAA), organs from Hepatitis-C (HCV) positive donors can be used for transplant in HCV-negative (HCV-) recipients with excellent graft survival and post-transplant course. This has expanded the donor pool to meet the accelerating need of liver transplantation in the United States. In trials involving HCV- recipients and HCV+ donors, up to 100% of the recipients achieved sustained virologic response using DAA therapy. However, the risk of HCV infection and subsequent hepatitis remained in certain patients.
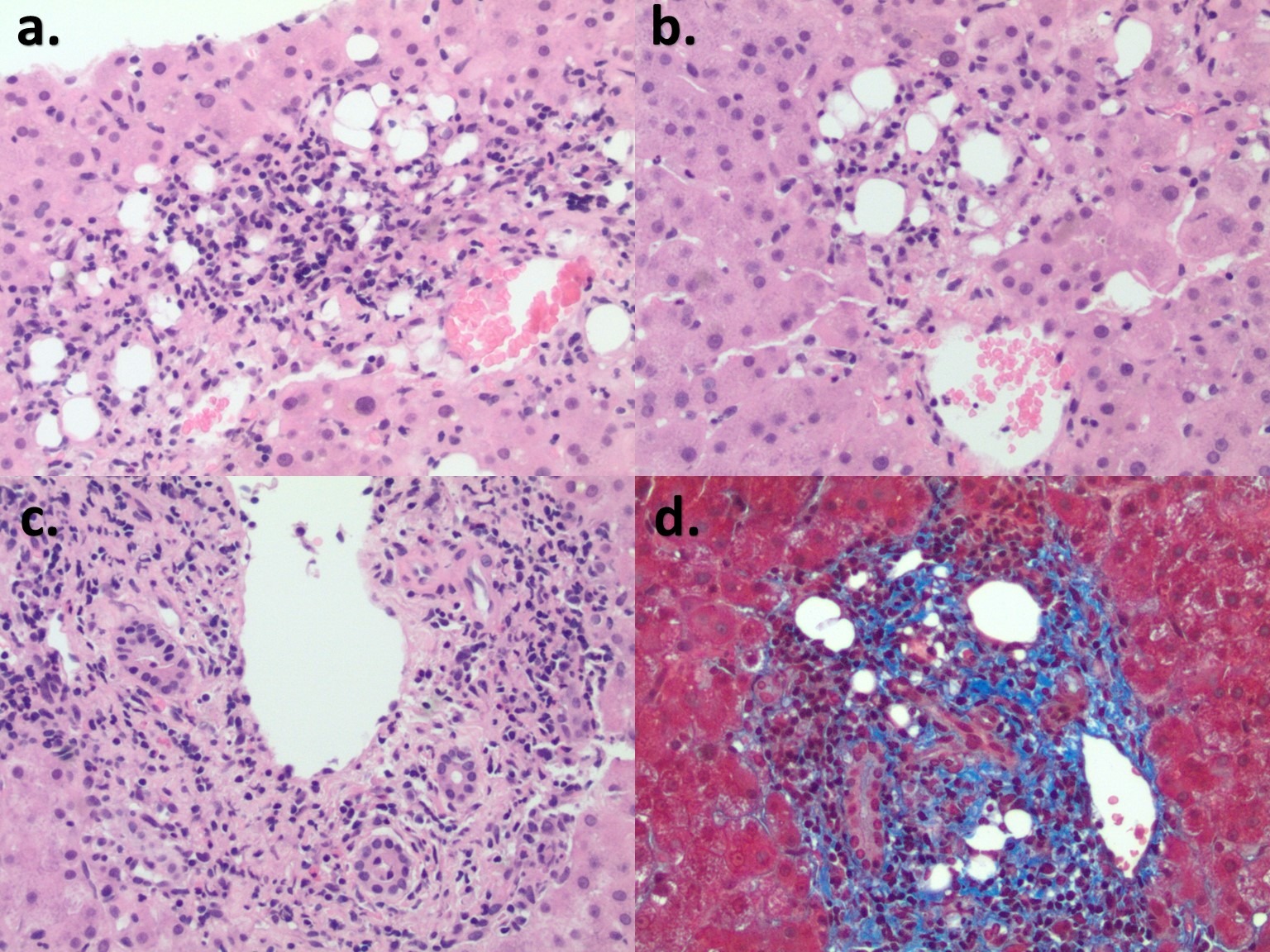
Case Description/Methods: We present a case of a 55-year-old male with a medical history of atrial fibrillation and hepatic cirrhosis secondary to primary biliary cholangitis, complicated by hepatocellular carcinoma. Pre-operative HCV antibody (ab) and RNA tests were negative for the recipient. He underwent successful orthotopic liver transplantation from a deceased donor that was HCV+. The post-transplantation course was complicated by undifferentiated shock, requiring vasopressors postoperative day (POD) 1, acute renal failure requiring dialysis POD 14, and persistent ascites complicated by multi-organism peritonitis. On POD 5, the patient had worsening hyperbilirubinemia, with a peak total bilirubin of 25.6 mg/dL on POD 12. A liver biopsy suggested mild acute cellular rejection but not fibrosing cholestatic hepatitis (FCH), which was inconsistent with the degree of hyperbilirubinemia. Histology revealed peri-portal lipogranulomas that are sometimes seen with early HCV-induced liver injury. The HCV RNA load was 25,863,636 IU/mL POD 7. The patient was started on Sofosbuvir / Velpatasvir for the treatment of HCV on POD 9. There was an improvement in HCV viral load (3,097 IU/mL POD 16), hyperbilirubinemia, and well shock.
Discussion: Acute HCV infection is rare and usually asymptomatic in immunocompetent patients; hence evidence regarding histologic appearance is limited. In post-transplant patients, HCV activation can mimic acute cellular rejection on pathology. It is recommended to start DAA within the first 7-14 days after clinical stability is achieved. Since the genotype of HCV from the donor is not routinely evaluated, it is recommended to use a pan-genotypic regimen (Glecaprevir/Pibrentasvir or Sofosbuvir/Velpatasvi). FCH is an important differential. Our patient did not have hepatitis C prior to the transplant, characteristic histopathologic findings, or a time course of more than 1 month after transplant as seen in FCH.
Disclosures:
Parth M. Patel, MD1, Hamna Fahad, MD2, Hassan Zreik, MD1, Zarqa Yasin, MD1, Mehak Bhatia, MD1, Syed-Mohammed Jafri, MD2. B0622 - A Case of Immediate Hepatitis C Infection Leading to Cholestatic Hepatitis With Significant Viremia After Liver Transplantation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Henry Ford Jackson, Jackson, MI; 2Henry Ford Health System, Detroit, MI
Introduction: With the success of direct active antiviral therapy (DAA), organs from Hepatitis-C (HCV) positive donors can be used for transplant in HCV-negative (HCV-) recipients with excellent graft survival and post-transplant course. This has expanded the donor pool to meet the accelerating need of liver transplantation in the United States. In trials involving HCV- recipients and HCV+ donors, up to 100% of the recipients achieved sustained virologic response using DAA therapy. However, the risk of HCV infection and subsequent hepatitis remained in certain patients.
Case Description/Methods: We present a case of a 55-year-old male with a medical history of atrial fibrillation and hepatic cirrhosis secondary to primary biliary cholangitis, complicated by hepatocellular carcinoma. Pre-operative HCV antibody (ab) and RNA tests were negative for the recipient. He underwent successful orthotopic liver transplantation from a deceased donor that was HCV+. The post-transplantation course was complicated by undifferentiated shock, requiring vasopressors postoperative day (POD) 1, acute renal failure requiring dialysis POD 14, and persistent ascites complicated by multi-organism peritonitis. On POD 5, the patient had worsening hyperbilirubinemia, with a peak total bilirubin of 25.6 mg/dL on POD 12. A liver biopsy suggested mild acute cellular rejection but not fibrosing cholestatic hepatitis (FCH), which was inconsistent with the degree of hyperbilirubinemia. Histology revealed peri-portal lipogranulomas that are sometimes seen with early HCV-induced liver injury. The HCV RNA load was 25,863,636 IU/mL POD 7. The patient was started on Sofosbuvir / Velpatasvir for the treatment of HCV on POD 9. There was an improvement in HCV viral load (3,097 IU/mL POD 16), hyperbilirubinemia, and well shock.
Discussion: Acute HCV infection is rare and usually asymptomatic in immunocompetent patients; hence evidence regarding histologic appearance is limited. In post-transplant patients, HCV activation can mimic acute cellular rejection on pathology. It is recommended to start DAA within the first 7-14 days after clinical stability is achieved. Since the genotype of HCV from the donor is not routinely evaluated, it is recommended to use a pan-genotypic regimen (Glecaprevir/Pibrentasvir or Sofosbuvir/Velpatasvi). FCH is an important differential. Our patient did not have hepatitis C prior to the transplant, characteristic histopathologic findings, or a time course of more than 1 month after transplant as seen in FCH.
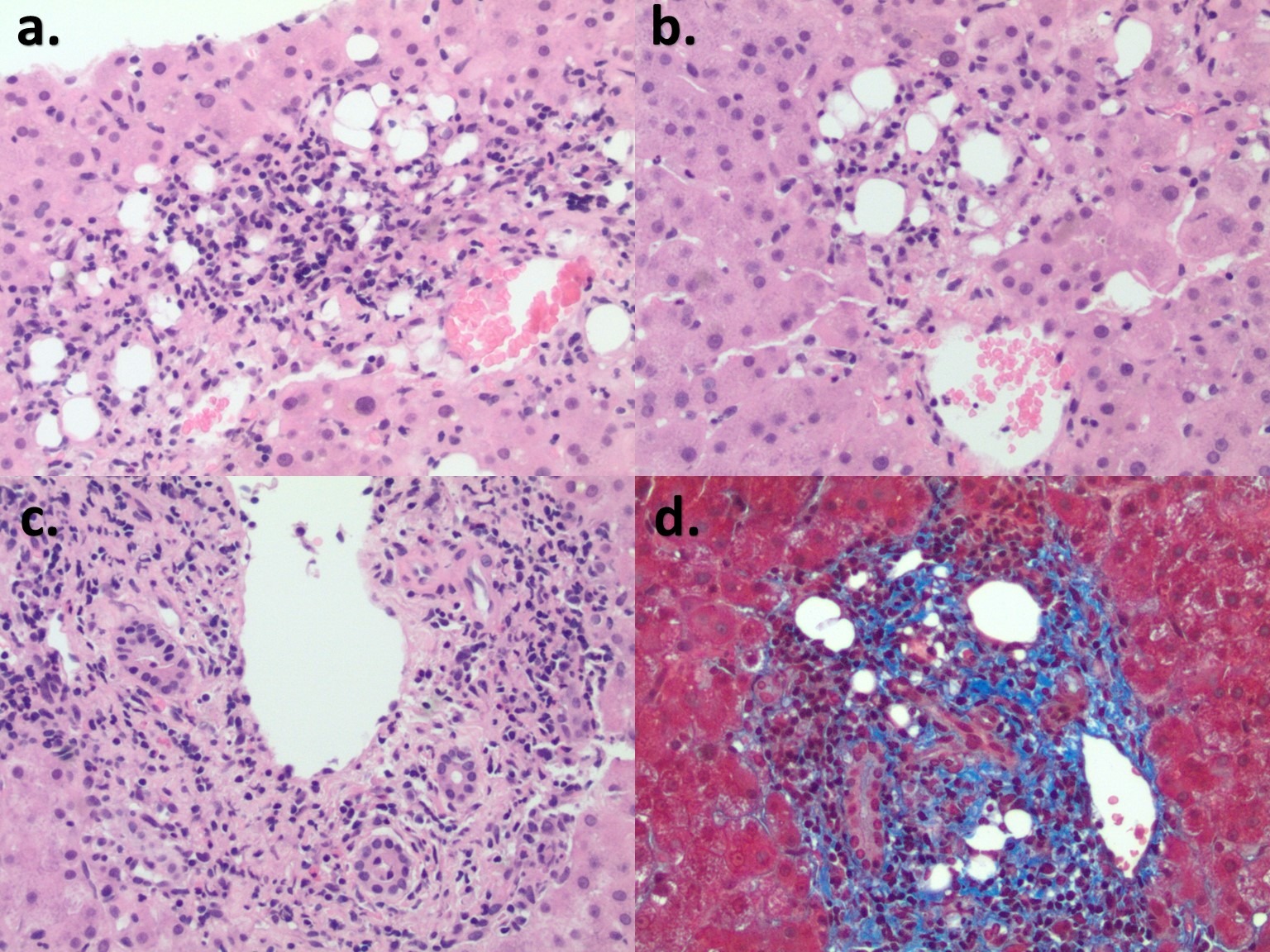
Figure: a & b. Some lipogranulomas are shown in portal tracts (left). In addition, hepatocyte focal necrosis evidenced by hepatocyte dropout and replaced with mononuclear cells and macrophages mixed with lipogranulomas are identified in the lobule (right). No dense lymphoid aggregate was identified, a typical feature for HCV. An unusual finding in acute cellular rejection, points to the recurrent HCV infection. c. Mild to focal moderate mixed inflammatory cell infiltrate seen in most portal tracts/areas, including neutrophils, mononuclear, eosinophils, and plasma cells, associated with scattered interface hepatitis. Focal endotheliitis is evidenced by inflammatory cells undermining the endothelial cells. Interlobular bile duct injury is focal and mild. Feature of Mild acute cellular rejection. d. Trichrome stain shows no delicate periportal strands of "chicken wire" like pericellular fibrosis; an early fibrosing cholestatic hepatitis is still under consideration.
Disclosures:
Parth Patel indicated no relevant financial relationships.
Hamna Fahad indicated no relevant financial relationships.
Hassan Zreik indicated no relevant financial relationships.
Zarqa Yasin indicated no relevant financial relationships.
Mehak Bhatia indicated no relevant financial relationships.
Mehak Bhatia — NO DISCLOSURE DATA.
Syed-Mohammed Jafri indicated no relevant financial relationships.
Parth M. Patel, MD1, Hamna Fahad, MD2, Hassan Zreik, MD1, Zarqa Yasin, MD1, Mehak Bhatia, MD1, Syed-Mohammed Jafri, MD2. B0622 - A Case of Immediate Hepatitis C Infection Leading to Cholestatic Hepatitis With Significant Viremia After Liver Transplantation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
