Back


Poster Session C - Monday Afternoon
Category: Colon
C0090 - Colitis on CT Imaging: Do the Radiographic Findings Correspond With Direct Visualization on Colonoscopy
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio
- CI
Chinonso Ilo, MD
Creighton University
Phoenix, AZ
Presenting Author(s)
Chinonso Ilo, MD1, Matthew Barvo, MD1, Hadiatou Barry, MD, MPH1, Venkata Pulivarthi, MD2, Subhash Chandra, MD1, Sarabdeep Mann, MD3, Bianca Varda, MD4
1Creighton University, Phoenix, AZ; 2Creighton University School of Medicine, Phoenix, AZ; 3Arizona Digestive Health, Phoenix, AZ; 4Loyola University Medical Center, Maywood, IL
Introduction: Patients present to the emergency department with complaints of abdominal pain at a higher frequency than any other ailment, according to the US Department of Health and Human Services. Healthcare providers will attempt to identify the root cause of patient's chief complaint, starting with physical exam, laboratory tests, and imaging studies. Performing a CT scan of the abdomen is a recommended choice. The scan may reveal inflammation, narrowing or thickening which allows the radiologist to suggest a diagnosis of colitis. However, there are limitations to the utility of imaging when diagnosing colitis. This study aims to identify if radiographic diagnosis of colitis corresponds to actual diagnosis of colitis when colonoscopy is done.
Methods: This study examined the results of CT imaging and colonoscopy of 50 patients who presented to the emergency department at a large, level-1 trauma center with chief complaint including abdominal pain and hematochezia. 30 women with an average age of 55 and 20 men with an average age of 59 were identified. Their CT abdomen suggested colitis per the radiologist’s interpretation. Upon that diagnosis, they had colonoscopy for definitive diagnosis. At the completion of their workup, data was analyzed.
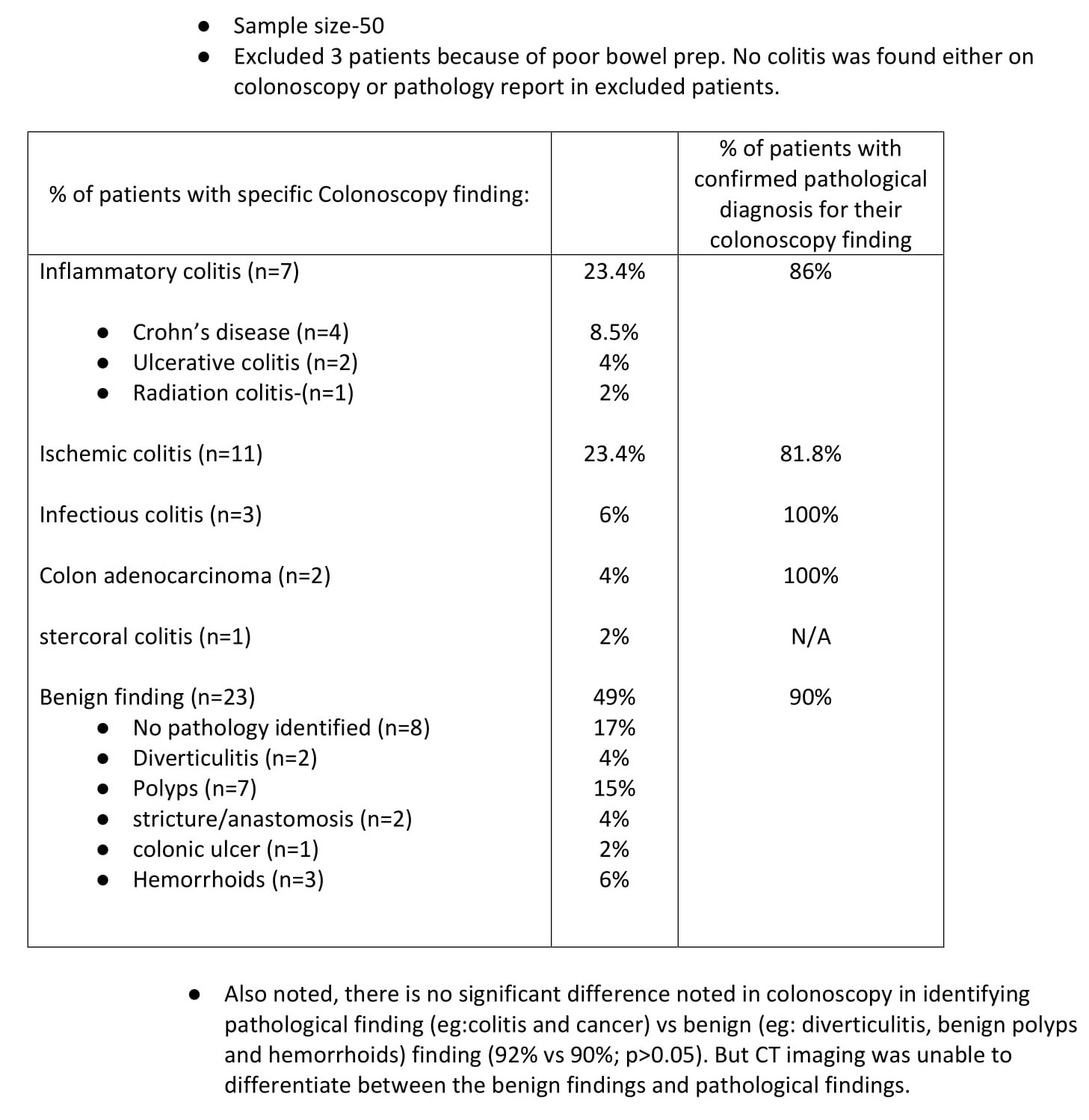
Results: Of the 50 patients examined, 47 patients with CT findings of colitis underwent colonoscopy. 22 (47%) had colitis on colonoscopy, 23 (49%) had no colitis on colonoscopy, 2 (4%) had colonic mass. Of the 22 patients with colitis on colonoscopy, 4 (8.5%) had Crohn’s disease, 2(4%) had Ulcerative colitis, 1 (2%) with radiation colitis, 11(23.4%) had ischemic colitis, 3 (6%) had infectious colitis, 1 (2%) had stercoral colitis. Pathology confirmed adenocarcinoma in the 2(4%) that had colonic mass. Of the 23 (48.9%%) with no colitis on colonoscopy, no pathology was identified in 8 (17%), 7 (15%) had benign polyps, 2 had diverticulitis (4%), 2 (4%) had stricture/anastomosis, 1 (2%) had colonic ulcer and 3(6%) had hemorrhoids. 86% of inflammatory colitis were confirmed by pathology, 81.8% of ischemic colitis was confirmed by pathology, infectious colitis and adenocarcinoma was confirmed 100% by pathology.
Discussion: Our study results illustrate a 49% false-positive rate of CT demonstrating colitis where colonoscopy findings were negative for colitis thus leading to overdiagnosis of colitis. Colonic mass/adenocarcinoma was missed on CT. This illustrates that colonoscopy remains the gold standard for diagnosis of colitis and tumors of gastrointestinal tract.
Disclosures:
Chinonso Ilo, MD1, Matthew Barvo, MD1, Hadiatou Barry, MD, MPH1, Venkata Pulivarthi, MD2, Subhash Chandra, MD1, Sarabdeep Mann, MD3, Bianca Varda, MD4. C0090 - Colitis on CT Imaging: Do the Radiographic Findings Correspond With Direct Visualization on Colonoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Creighton University, Phoenix, AZ; 2Creighton University School of Medicine, Phoenix, AZ; 3Arizona Digestive Health, Phoenix, AZ; 4Loyola University Medical Center, Maywood, IL
Introduction: Patients present to the emergency department with complaints of abdominal pain at a higher frequency than any other ailment, according to the US Department of Health and Human Services. Healthcare providers will attempt to identify the root cause of patient's chief complaint, starting with physical exam, laboratory tests, and imaging studies. Performing a CT scan of the abdomen is a recommended choice. The scan may reveal inflammation, narrowing or thickening which allows the radiologist to suggest a diagnosis of colitis. However, there are limitations to the utility of imaging when diagnosing colitis. This study aims to identify if radiographic diagnosis of colitis corresponds to actual diagnosis of colitis when colonoscopy is done.
Methods: This study examined the results of CT imaging and colonoscopy of 50 patients who presented to the emergency department at a large, level-1 trauma center with chief complaint including abdominal pain and hematochezia. 30 women with an average age of 55 and 20 men with an average age of 59 were identified. Their CT abdomen suggested colitis per the radiologist’s interpretation. Upon that diagnosis, they had colonoscopy for definitive diagnosis. At the completion of their workup, data was analyzed.
Results: Of the 50 patients examined, 47 patients with CT findings of colitis underwent colonoscopy. 22 (47%) had colitis on colonoscopy, 23 (49%) had no colitis on colonoscopy, 2 (4%) had colonic mass. Of the 22 patients with colitis on colonoscopy, 4 (8.5%) had Crohn’s disease, 2(4%) had Ulcerative colitis, 1 (2%) with radiation colitis, 11(23.4%) had ischemic colitis, 3 (6%) had infectious colitis, 1 (2%) had stercoral colitis. Pathology confirmed adenocarcinoma in the 2(4%) that had colonic mass. Of the 23 (48.9%%) with no colitis on colonoscopy, no pathology was identified in 8 (17%), 7 (15%) had benign polyps, 2 had diverticulitis (4%), 2 (4%) had stricture/anastomosis, 1 (2%) had colonic ulcer and 3(6%) had hemorrhoids. 86% of inflammatory colitis were confirmed by pathology, 81.8% of ischemic colitis was confirmed by pathology, infectious colitis and adenocarcinoma was confirmed 100% by pathology.
Discussion: Our study results illustrate a 49% false-positive rate of CT demonstrating colitis where colonoscopy findings were negative for colitis thus leading to overdiagnosis of colitis. Colonic mass/adenocarcinoma was missed on CT. This illustrates that colonoscopy remains the gold standard for diagnosis of colitis and tumors of gastrointestinal tract.
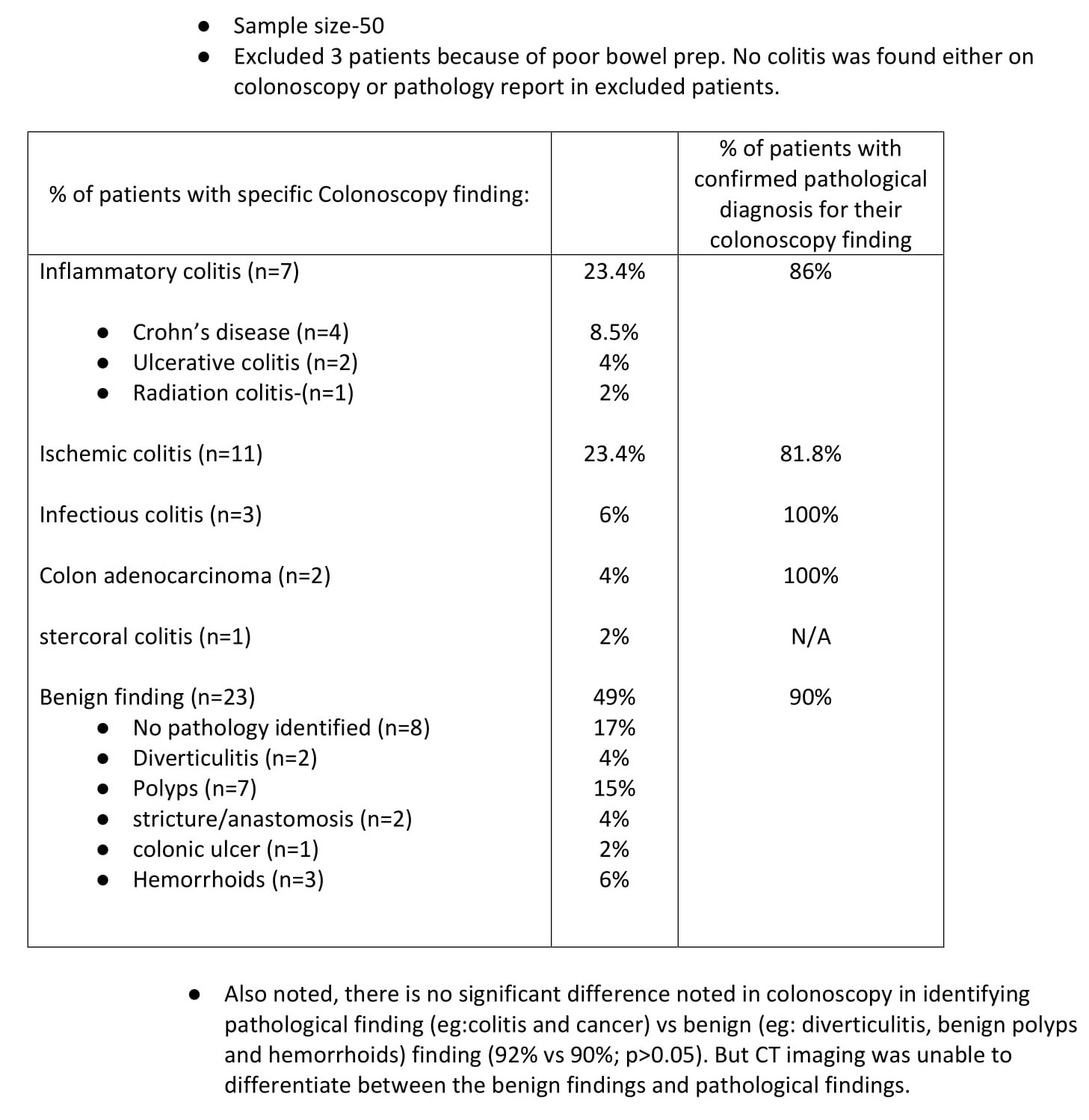
Figure: Image 1
Disclosures:
Chinonso Ilo indicated no relevant financial relationships.
Matthew Barvo indicated no relevant financial relationships.
Hadiatou Barry indicated no relevant financial relationships.
Venkata Pulivarthi indicated no relevant financial relationships.
Subhash Chandra indicated no relevant financial relationships.
Sarabdeep Mann indicated no relevant financial relationships.
Bianca Varda indicated no relevant financial relationships.
Chinonso Ilo, MD1, Matthew Barvo, MD1, Hadiatou Barry, MD, MPH1, Venkata Pulivarthi, MD2, Subhash Chandra, MD1, Sarabdeep Mann, MD3, Bianca Varda, MD4. C0090 - Colitis on CT Imaging: Do the Radiographic Findings Correspond With Direct Visualization on Colonoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
