Back

Poster Session A - Sunday Afternoon
Category: GI Bleeding
A0327 - Three Simultaneous Sources of Upper GI Bleeding
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Herman Suga, DO
Jefferson Health New Jersey
Turnersville, NJ
Presenting Author(s)
David J. Truscello, DO1, Seth H. Lipshutz, DO2, Herman Suga, DO1, Richard Walters, DO1
1Jefferson Health New Jersey, Turnersville, NJ; 2Jefferson Health Northeast, Philadelphia, PA
Introduction: Acute upper GI bleeding is one of the most common causes of gastrointestinal related hospitalizations. Presentation of these patients commonly includes melena, hematemesis, or unstable hematochezia. One of the most common etiologies for this presentation is peptic ulcer disease. However less common causes include Dieulafoy lesions and iatrogenic gastric fistulas. The following case discusses three simultaneously diagnosed causes of upper GI bleeding.
Case Description/Methods: An 82-year-old male with a history of splenectomy presented with melena and syncope. The day of arrival patient had syncopized after having multiple large bouts of black stool. On presentation, he was hypotensive, and tachycardic. His hemoglobin was 6.3 g/dL with a BUN of 62 mg/dL. An EGD was planned following patient stabilization. Initial EGD revealed a single 8mm ulcer in the duodenal bulb with no stigmata of bleeding. Just distally to the ulcer in the duodenal sweep was an actively bleeding Dieulafoy lesion. Hemostasis was achieved with bipolar cautery and the active bleed was stopped. Retroflexion during the initial procedure showed retained clot and old blood in the fundus that was presumed from the Dieulafoy lesion. Despite intervention, patient continued to have large bouts of melena the evening after the procedure. A 2nd EGD was performed and showed a stable ulcer and no signs of recurrent Dieulafoy. The fundus was now more visible and revealed ischemic damage. Careful inspection revealed a fistula with suture material free floating. Review of the operative note from the splenectomy revealed patient suffered a small laceration to the gastric fundus during the procedure which was repaired with an inner row of sutures. Given the size of the fistula, decision made for a CT scan to better define the anatomy. Unfortunately, the patient continued to decompensate, and family ultimately elected for comfort care.
Discussion: Dieulafoy lesions and gastric fistulas are both relatively rare, but potentially life-threatening, conditions. A Dieulafoy is a narrow artery that bleeds through a small mucosal defect. Therapeutic endoscopy can control the bleeding in 90% of patients while angiography is being accepted as an alternative to endoscopy for inaccessible lesions. The most common site for a Dieulafoy lesion to appear is in the lesser curvature. Gastric fistulas status post splenectomy occur in less than 1% of cases with the usual site along the greater curvature near the fundus.
Disclosures:
David J. Truscello, DO1, Seth H. Lipshutz, DO2, Herman Suga, DO1, Richard Walters, DO1. A0327 - Three Simultaneous Sources of Upper GI Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Jefferson Health New Jersey, Turnersville, NJ; 2Jefferson Health Northeast, Philadelphia, PA
Introduction: Acute upper GI bleeding is one of the most common causes of gastrointestinal related hospitalizations. Presentation of these patients commonly includes melena, hematemesis, or unstable hematochezia. One of the most common etiologies for this presentation is peptic ulcer disease. However less common causes include Dieulafoy lesions and iatrogenic gastric fistulas. The following case discusses three simultaneously diagnosed causes of upper GI bleeding.
Case Description/Methods: An 82-year-old male with a history of splenectomy presented with melena and syncope. The day of arrival patient had syncopized after having multiple large bouts of black stool. On presentation, he was hypotensive, and tachycardic. His hemoglobin was 6.3 g/dL with a BUN of 62 mg/dL. An EGD was planned following patient stabilization. Initial EGD revealed a single 8mm ulcer in the duodenal bulb with no stigmata of bleeding. Just distally to the ulcer in the duodenal sweep was an actively bleeding Dieulafoy lesion. Hemostasis was achieved with bipolar cautery and the active bleed was stopped. Retroflexion during the initial procedure showed retained clot and old blood in the fundus that was presumed from the Dieulafoy lesion. Despite intervention, patient continued to have large bouts of melena the evening after the procedure. A 2nd EGD was performed and showed a stable ulcer and no signs of recurrent Dieulafoy. The fundus was now more visible and revealed ischemic damage. Careful inspection revealed a fistula with suture material free floating. Review of the operative note from the splenectomy revealed patient suffered a small laceration to the gastric fundus during the procedure which was repaired with an inner row of sutures. Given the size of the fistula, decision made for a CT scan to better define the anatomy. Unfortunately, the patient continued to decompensate, and family ultimately elected for comfort care.
Discussion: Dieulafoy lesions and gastric fistulas are both relatively rare, but potentially life-threatening, conditions. A Dieulafoy is a narrow artery that bleeds through a small mucosal defect. Therapeutic endoscopy can control the bleeding in 90% of patients while angiography is being accepted as an alternative to endoscopy for inaccessible lesions. The most common site for a Dieulafoy lesion to appear is in the lesser curvature. Gastric fistulas status post splenectomy occur in less than 1% of cases with the usual site along the greater curvature near the fundus.
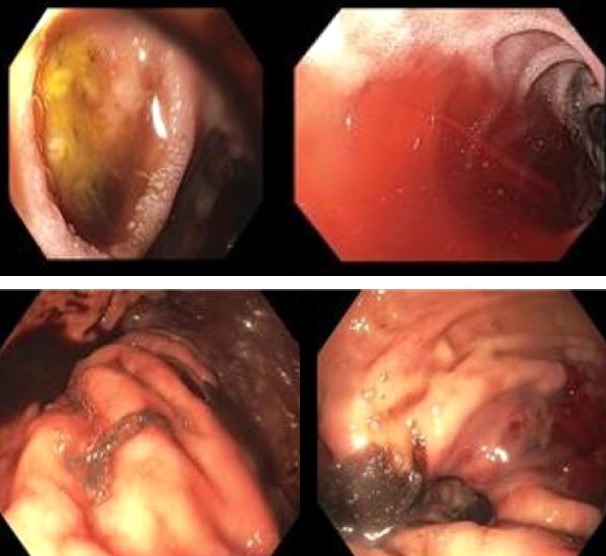
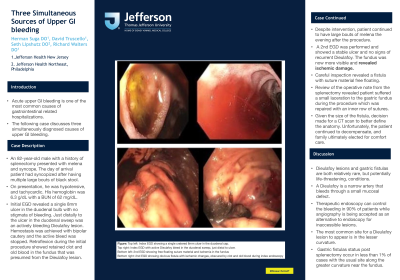
Figure: Top left: Index EGD showing a single cratered 8mm ulcer in the duodenal cap.
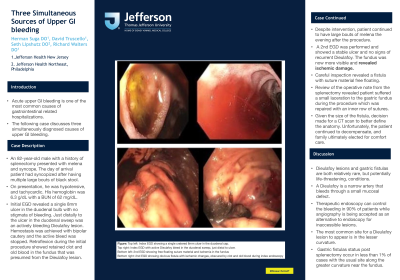
Top right: Index EGD with active Dieulafoy bleed in the duodenal sweep, just distal to ulcer.
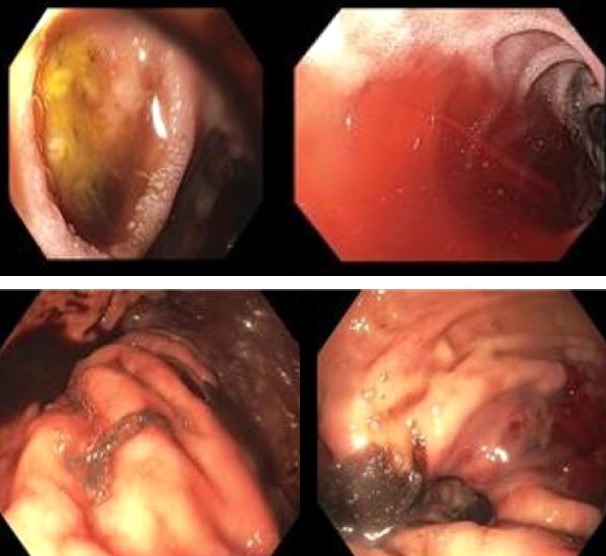
Bottom left: 2nd EGD showing free floating suture material and ischemia in the fundus
Bottom right: 2nd EGD showing obvious fistula with ischemic changes, obscured by clot and old blood during index endoscopy
Top right: Index EGD with active Dieulafoy bleed in the duodenal sweep, just distal to ulcer.
Bottom left: 2nd EGD showing free floating suture material and ischemia in the fundus
Bottom right: 2nd EGD showing obvious fistula with ischemic changes, obscured by clot and old blood during index endoscopy
Disclosures:
David Truscello indicated no relevant financial relationships.
Seth Lipshutz indicated no relevant financial relationships.
Herman Suga indicated no relevant financial relationships.
Richard Walters indicated no relevant financial relationships.
David J. Truscello, DO1, Seth H. Lipshutz, DO2, Herman Suga, DO1, Richard Walters, DO1. A0327 - Three Simultaneous Sources of Upper GI Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
