Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0346 - An Unusual Case of Massive Upper Gastrointestinal Bleeding: HSV Esophagitis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Christina Gomez, MD
University of Missouri Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Christina Gomez, MD1, Daniel Merrill, DO, MBA2, Laith Al Momani, MD1, Wendell Clarkston, MD3
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2University of Missouri-Kansas City School of Medicine, Kansas City, MO; 3University of Missouri-Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO
Introduction: Herpes simplex virus (HSV) esophagitis is more commonly diagnosed in immunocompromised patients and generally presents with acute onset dysphagia and odynophagia. We discuss a case of HSV esophagitis in an immunocompetent patient presenting with massive GI bleeding without dysphagia or odynophagia.
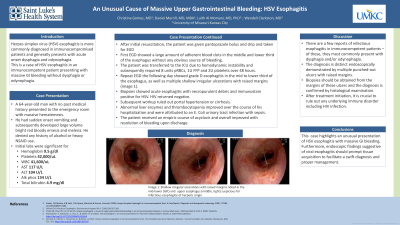
Case Description/Methods: A 64-year-old man with no past medical history presented to the emergency room with massive hematemesis. He had sudden onset vomiting and subsequently developed large volume bright red bloody emesis and melena. He denied any history of alcohol or heavy NSAID use. Labs were significant for anemia (hgb 9.5 g/dl), thrombocytopenia (plts 42k x10E3/uL), leukocytosis (WBC 41.6 x10E3/uL), elevated liver tests (AST 117 U/L and ALT 104 U/L, ALP 134 U/L, total bilirubin 4.9 mg/dl). After initial resuscitation, the patient was given pantoprazole bolus and drip and taken for EGD which showed a large amount of adherent blood clots in the middle and lower third of the esophagus without any obvious source of bleeding. The patient was transferred to the ICU due to hemodynamic instability and subsequently required 8 units pRBCs, 1U FFP and 2U plts over 48 hours. Repeat EGD the following day showed grade D esophagitis in the mid to lower third of the esophagus, as well as multiple shallow irregular ulcerations with raised margins. Biopsies showed acute esophagitis with necropurulent debris and immunostain positive for HSV. HIV returned negative. Subsequent workup ruled out portal hypertension or cirrhosis. Abnormal liver enzymes and thrombocytopenia improved over the course of his hospitalization and were attributed to E. Coli urinary tract infection with sepsis. The patient received an empiric course of acyclovir and overall improved with resolution of bleeding upon discharge.
Discussion: There are a few reports of infectious esophagitis in immunocompetent patients that most commonly present with dysphagia and odynophagia. The diagnosis is distinct endoscopically by multiple punched-out ulcers with raised margins. Biopsies should be obtained from the margins of these ulcers and the diagnosis is then confirmed by histological examination. After treatment initiation, it is crucial to rule out any underlying immune disorder including HIV infection. Our case highlights an unusual presentation of HSV esophagitis with massive GI bleeding. Furthermore, endoscopic findings suggestive of viral esophagitis should prompt tissue acquisition to facilitate a swift diagnosis and proper management.

Disclosures:
Christina Gomez, MD1, Daniel Merrill, DO, MBA2, Laith Al Momani, MD1, Wendell Clarkston, MD3. B0346 - An Unusual Case of Massive Upper Gastrointestinal Bleeding: HSV Esophagitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2University of Missouri-Kansas City School of Medicine, Kansas City, MO; 3University of Missouri-Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO
Introduction: Herpes simplex virus (HSV) esophagitis is more commonly diagnosed in immunocompromised patients and generally presents with acute onset dysphagia and odynophagia. We discuss a case of HSV esophagitis in an immunocompetent patient presenting with massive GI bleeding without dysphagia or odynophagia.
Case Description/Methods: A 64-year-old man with no past medical history presented to the emergency room with massive hematemesis. He had sudden onset vomiting and subsequently developed large volume bright red bloody emesis and melena. He denied any history of alcohol or heavy NSAID use. Labs were significant for anemia (hgb 9.5 g/dl), thrombocytopenia (plts 42k x10E3/uL), leukocytosis (WBC 41.6 x10E3/uL), elevated liver tests (AST 117 U/L and ALT 104 U/L, ALP 134 U/L, total bilirubin 4.9 mg/dl). After initial resuscitation, the patient was given pantoprazole bolus and drip and taken for EGD which showed a large amount of adherent blood clots in the middle and lower third of the esophagus without any obvious source of bleeding. The patient was transferred to the ICU due to hemodynamic instability and subsequently required 8 units pRBCs, 1U FFP and 2U plts over 48 hours. Repeat EGD the following day showed grade D esophagitis in the mid to lower third of the esophagus, as well as multiple shallow irregular ulcerations with raised margins. Biopsies showed acute esophagitis with necropurulent debris and immunostain positive for HSV. HIV returned negative. Subsequent workup ruled out portal hypertension or cirrhosis. Abnormal liver enzymes and thrombocytopenia improved over the course of his hospitalization and were attributed to E. Coli urinary tract infection with sepsis. The patient received an empiric course of acyclovir and overall improved with resolution of bleeding upon discharge.
Discussion: There are a few reports of infectious esophagitis in immunocompetent patients that most commonly present with dysphagia and odynophagia. The diagnosis is distinct endoscopically by multiple punched-out ulcers with raised margins. Biopsies should be obtained from the margins of these ulcers and the diagnosis is then confirmed by histological examination. After treatment initiation, it is crucial to rule out any underlying immune disorder including HIV infection. Our case highlights an unusual presentation of HSV esophagitis with massive GI bleeding. Furthermore, endoscopic findings suggestive of viral esophagitis should prompt tissue acquisition to facilitate a swift diagnosis and proper management.

Figure: Image 1: Shallow irregular ulcerations with raised margins noted in the upper esophagus suspicious for infectious esophagitis of herpetic origin
Disclosures:
Christina Gomez indicated no relevant financial relationships.
Daniel Merrill indicated no relevant financial relationships.
Laith Al Momani indicated no relevant financial relationships.
Wendell Clarkston indicated no relevant financial relationships.
Christina Gomez, MD1, Daniel Merrill, DO, MBA2, Laith Al Momani, MD1, Wendell Clarkston, MD3. B0346 - An Unusual Case of Massive Upper Gastrointestinal Bleeding: HSV Esophagitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
