Back

Poster Session C - Monday Afternoon
Category: GI Bleeding
C0329 - Endoscopic Approaches to the Management of Blue Rubber Bleb Nevus Syndrome
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Hammad Qureshi, MD
University of Kentucky
Lexington, KY
Presenting Author(s)
Hammad Qureshi, MD1, Naba Saeed, MD2, Nimish Thakral, MD1, Samuel Mardini, MD, MBA, MPH, FACG1, Deborah Flomenhoft, MD1
1University of Kentucky, Lexington, KY; 2The University of Kentucky, Lexington, KY
Introduction: Blue rubber bleb nevus syndrome (BRBNS) is a rare but potentially life-threatening disorder characterized by cutaneous and gastrointestinal tract vascular malformations and chronic iron deficiency anemia. Patients present on a spectrum from mild anemia to severe hemorrhage or even intestinal obstruction/intussusception. No standard of care exists for therapy in these patients, and the optimal endoscopic technique for management of arteriovenous malformation (AVM) related bleeding has not been elucidated. Here we present a case illustrating successes of different endoscopic therapies for BRBNS.
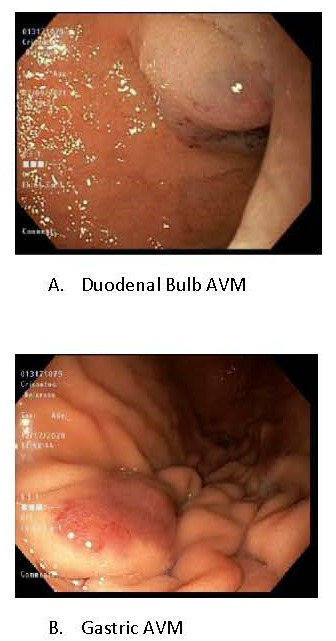
Case Description/Methods: A 23 year old lady , diagnosed in her teens with BRBNS, with resultant anemia and bowel obstructions due to AVMs, s/p resections, painful palmar and gluteal lesions s/p resection and digital amputations, presented to discuss therapies for her GI AVMs. Was started on sirolimus by hematology, but unable to take it regularly due to social/financial constraints. EGD 12/17/2020 with gastric and duodenal submucosal blebs/hemangiomas; banded x2. Diagnosis was confirmed with EUS, Hemoglobin (Hb) was 8.8. The next day, she developed hematemesis/ melena with Hb drop to 5.7. Repeat EGD: post banding ulcers with pigmented material in the gastric body, s/p Argon plasma coagulation. Hb stabilized and patient was discharged. Subsequently, did not have signs of overt GI Bleeding. Upon follow up EGD 02/’21, performed hemostatic injection (with sodium tetradecyl sulphate) of persistent duodenal lesions. In conjunction with this, she was taking her sirolimus more regularly. Subsequently her Hb has uptrended with no further overt bleeding in over a year.
Discussion: Management strategies for BRBNS include antiangiogenic therapies, endoscopic treatments, and even surgical resection. Reports from 1990 to date have described benefit with sirolimus therapy + pre-emptive endoscopic treatment with bipolar cautery, APC, band ligation and sclerosing/hemostatic injection. Surgery is usually reserved as a last resort as lesions can reappear elsewhere along the GI tract. In our patient, due to cost of antiangiogenic treatment, finding an endoscopic approach that worked for her was prudent. Although band ligation was attempted, the resultant bleeding from post-banding ulcers seemed to be even worse than her baseline slow rate of bleeding. Hemostatic injection appeared to be an effective measure for her in tandem with sirolimus therapy.
Disclosures:
Hammad Qureshi, MD1, Naba Saeed, MD2, Nimish Thakral, MD1, Samuel Mardini, MD, MBA, MPH, FACG1, Deborah Flomenhoft, MD1. C0329 - Endoscopic Approaches to the Management of Blue Rubber Bleb Nevus Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2The University of Kentucky, Lexington, KY
Introduction: Blue rubber bleb nevus syndrome (BRBNS) is a rare but potentially life-threatening disorder characterized by cutaneous and gastrointestinal tract vascular malformations and chronic iron deficiency anemia. Patients present on a spectrum from mild anemia to severe hemorrhage or even intestinal obstruction/intussusception. No standard of care exists for therapy in these patients, and the optimal endoscopic technique for management of arteriovenous malformation (AVM) related bleeding has not been elucidated. Here we present a case illustrating successes of different endoscopic therapies for BRBNS.
Case Description/Methods: A 23 year old lady , diagnosed in her teens with BRBNS, with resultant anemia and bowel obstructions due to AVMs, s/p resections, painful palmar and gluteal lesions s/p resection and digital amputations, presented to discuss therapies for her GI AVMs. Was started on sirolimus by hematology, but unable to take it regularly due to social/financial constraints. EGD 12/17/2020 with gastric and duodenal submucosal blebs/hemangiomas; banded x2. Diagnosis was confirmed with EUS, Hemoglobin (Hb) was 8.8. The next day, she developed hematemesis/ melena with Hb drop to 5.7. Repeat EGD: post banding ulcers with pigmented material in the gastric body, s/p Argon plasma coagulation. Hb stabilized and patient was discharged. Subsequently, did not have signs of overt GI Bleeding. Upon follow up EGD 02/’21, performed hemostatic injection (with sodium tetradecyl sulphate) of persistent duodenal lesions. In conjunction with this, she was taking her sirolimus more regularly. Subsequently her Hb has uptrended with no further overt bleeding in over a year.
Discussion: Management strategies for BRBNS include antiangiogenic therapies, endoscopic treatments, and even surgical resection. Reports from 1990 to date have described benefit with sirolimus therapy + pre-emptive endoscopic treatment with bipolar cautery, APC, band ligation and sclerosing/hemostatic injection. Surgery is usually reserved as a last resort as lesions can reappear elsewhere along the GI tract. In our patient, due to cost of antiangiogenic treatment, finding an endoscopic approach that worked for her was prudent. Although band ligation was attempted, the resultant bleeding from post-banding ulcers seemed to be even worse than her baseline slow rate of bleeding. Hemostatic injection appeared to be an effective measure for her in tandem with sirolimus therapy.
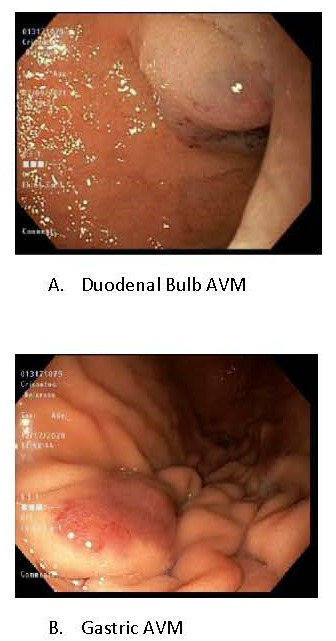
Figure: Numerous large AVMs dispersed throughout the Upper GI tract
Disclosures:
Hammad Qureshi indicated no relevant financial relationships.
Naba Saeed indicated no relevant financial relationships.
Nimish Thakral indicated no relevant financial relationships.
Samuel Mardini indicated no relevant financial relationships.
Deborah Flomenhoft indicated no relevant financial relationships.
Hammad Qureshi, MD1, Naba Saeed, MD2, Nimish Thakral, MD1, Samuel Mardini, MD, MBA, MPH, FACG1, Deborah Flomenhoft, MD1. C0329 - Endoscopic Approaches to the Management of Blue Rubber Bleb Nevus Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
