Back

Poster Session A - Sunday Afternoon
Category: IBD
A0407 - Isolated Celiac Artery Vasculitis Presenting as Ileus in a Patient With Ulcerative Colitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Sareena Ali, DO
Advocate Lutheran General Hospital
Park Ridge, IL
Presenting Author(s)
Sareena Ali, DO1, Meghana Doniparthi, MD1, Nahren Asado, MD1, Kristina Borgen, MD1, Alan Shapiro, MD, FACG2
1Advocate Lutheran General Hospital, Park Ridge, IL; 2Advocate Lutheran General Hospital, Glenview, IL
Introduction: Small case series have reported an association between IBD and large vessel vasculitides, ANCA-associated vasculitis, and cutaneous vasculitis. Gastrointestinal (GI) involvement of vasculitis can be a severe complication, resulting in mesenteric ischemia, ileus, or GI bleeding, and often requires aggressive medical or surgical interventions. We report a case of celiac artery vasculitis presenting as abdominal pain and ileus in a patient with ulcerative colitis (UC).
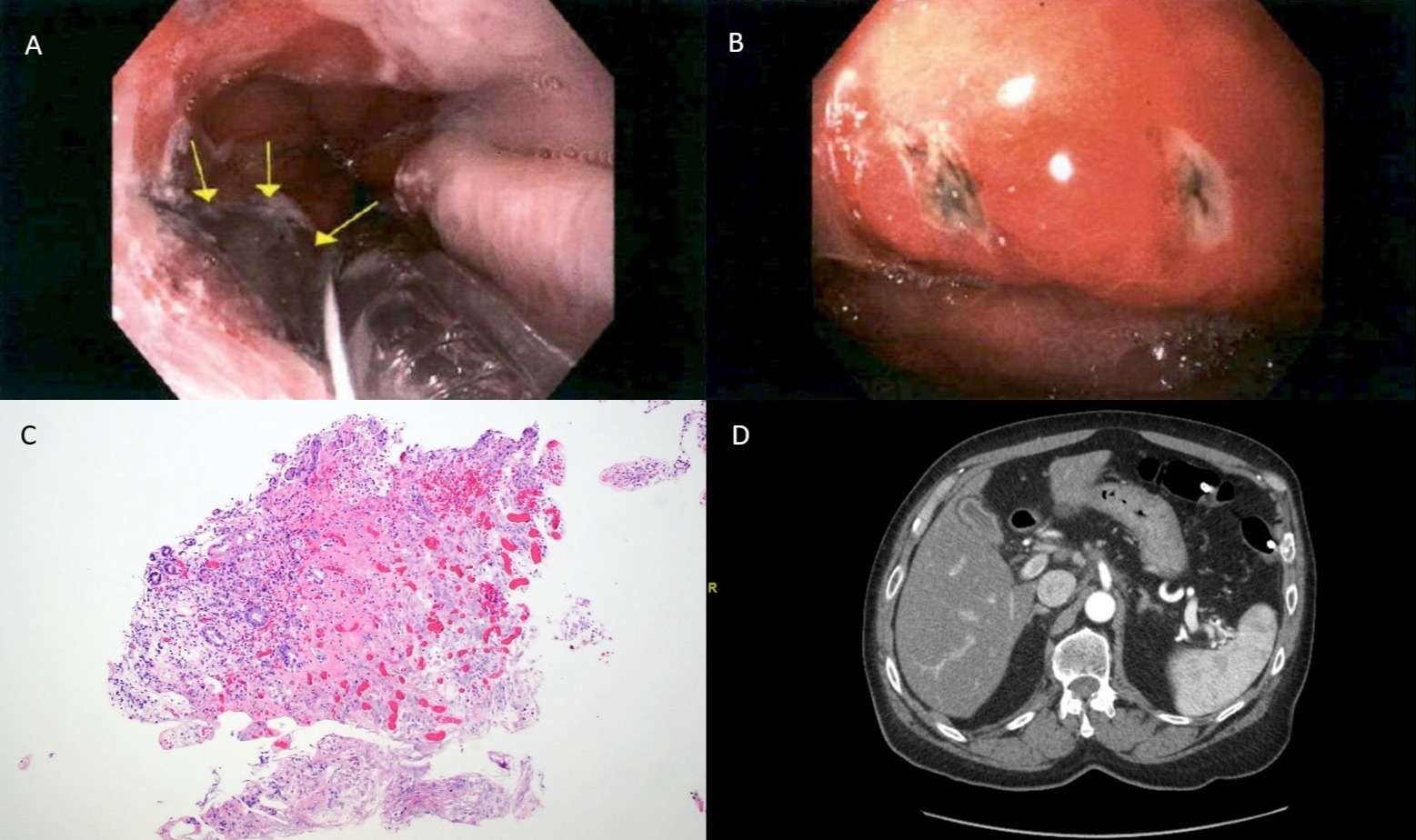
Case Description/Methods: A 69 year old male with an 11 year history of UC in remission on infliximab and azathioprine (AZA) presented to the emergency room with abdominal pain and constipation for five days. He had decreased AZA from 200 mg to 100 mg one month prior. Initial CT abdomen and pelvis showed stranding surrounding the celiac artery, fluid-filled small bowel loops, and segmental areas of distal colon collapse with proximal colon distention. He developed progressive small bowel and colonic distention with cecum diameter of 10 cm. A colonoscopy was performed for decompression. He had no evidence of active UC. EGD demonstrated dusky appearing gastroesophageal junction and inflammation with cratered ulcers in the gastric cardia and body. Biopsies confirmed ischemic necrosis. CTA demonstrated perivascular inflammation of a patent celiac artery without evidence for dissection, suggestive of acute vasculitis. ESR and CRP were 50 mm/hr and 7.8 mg/dL respectively. Myeloperoxidase, serine-proteinase 3, rheumatoid factor, ANA, were negative. He was started on methylprednisolone IV with oral prednisone taper at discharge, and AZA was increased to 200 mg daily. A CT one month later showed minimal residual inflammation. ESR and CRP had normalized.
Discussion: We present the first case of isolated celiac artery vasculitis in a patient with IBD. A diagnosis of IBD often precedes vasculitis, and patients are typically on immunosuppressive therapy at the time of onset. Anti-TNF agents have been implicated as a potential inciting cause. Although it is unclear whether long-term anti-TNF therapy precipitated vasculitis in our patient, the dose reduction in AZA prior to presentation may have unmasked vasculitis. This was supported by his rapid clinical and radiographic improvement with combination of steroids and increased AZA dose despite continuation of infliximab. This case highlights the importance of maintaining a high degree of suspicion for vasculitis in patients with IBD on immunosuppressive therapy presenting with ischemia or ileus.
Disclosures:
Sareena Ali, DO1, Meghana Doniparthi, MD1, Nahren Asado, MD1, Kristina Borgen, MD1, Alan Shapiro, MD, FACG2. A0407 - Isolated Celiac Artery Vasculitis Presenting as Ileus in a Patient With Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Advocate Lutheran General Hospital, Park Ridge, IL; 2Advocate Lutheran General Hospital, Glenview, IL
Introduction: Small case series have reported an association between IBD and large vessel vasculitides, ANCA-associated vasculitis, and cutaneous vasculitis. Gastrointestinal (GI) involvement of vasculitis can be a severe complication, resulting in mesenteric ischemia, ileus, or GI bleeding, and often requires aggressive medical or surgical interventions. We report a case of celiac artery vasculitis presenting as abdominal pain and ileus in a patient with ulcerative colitis (UC).
Case Description/Methods: A 69 year old male with an 11 year history of UC in remission on infliximab and azathioprine (AZA) presented to the emergency room with abdominal pain and constipation for five days. He had decreased AZA from 200 mg to 100 mg one month prior. Initial CT abdomen and pelvis showed stranding surrounding the celiac artery, fluid-filled small bowel loops, and segmental areas of distal colon collapse with proximal colon distention. He developed progressive small bowel and colonic distention with cecum diameter of 10 cm. A colonoscopy was performed for decompression. He had no evidence of active UC. EGD demonstrated dusky appearing gastroesophageal junction and inflammation with cratered ulcers in the gastric cardia and body. Biopsies confirmed ischemic necrosis. CTA demonstrated perivascular inflammation of a patent celiac artery without evidence for dissection, suggestive of acute vasculitis. ESR and CRP were 50 mm/hr and 7.8 mg/dL respectively. Myeloperoxidase, serine-proteinase 3, rheumatoid factor, ANA, were negative. He was started on methylprednisolone IV with oral prednisone taper at discharge, and AZA was increased to 200 mg daily. A CT one month later showed minimal residual inflammation. ESR and CRP had normalized.
Discussion: We present the first case of isolated celiac artery vasculitis in a patient with IBD. A diagnosis of IBD often precedes vasculitis, and patients are typically on immunosuppressive therapy at the time of onset. Anti-TNF agents have been implicated as a potential inciting cause. Although it is unclear whether long-term anti-TNF therapy precipitated vasculitis in our patient, the dose reduction in AZA prior to presentation may have unmasked vasculitis. This was supported by his rapid clinical and radiographic improvement with combination of steroids and increased AZA dose despite continuation of infliximab. This case highlights the importance of maintaining a high degree of suspicion for vasculitis in patients with IBD on immunosuppressive therapy presenting with ischemia or ileus.
Figure: Figure 1: A 69 year old male underwent EGD for evaluation of abdominal pain and NG tube placement; he was found to have inflammation with a dusky appearing mucosa at the gastroesophageal junction (GEJ) (A). Non-bleeding gastric ulcers with overlying pigment (Forrest Class IIc) were identified (B). H&E stain image shows the GEJ biopsy with extensive ischemic necrosis and hemorrhage (C). Initial CTA abdomen/pelvis shows fat stranding surrounding the celiac artery (D).
Disclosures:
Sareena Ali indicated no relevant financial relationships.
Meghana Doniparthi indicated no relevant financial relationships.
Nahren Asado indicated no relevant financial relationships.
Kristina Borgen indicated no relevant financial relationships.
Alan Shapiro indicated no relevant financial relationships.
Sareena Ali, DO1, Meghana Doniparthi, MD1, Nahren Asado, MD1, Kristina Borgen, MD1, Alan Shapiro, MD, FACG2. A0407 - Isolated Celiac Artery Vasculitis Presenting as Ileus in a Patient With Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

