Back

Poster Session D - Tuesday Morning
Category: Stomach
D0691 - Effects of Surgical Pyloroplasty on Pyloric EndoFLIP Measurements and Gastric Emptying in Patients With Refractory Gastroparesis and Identification of Pyloric Sphincter Smooth Muscle Pathology
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Andrew J. Ortega, DO
Texas Tech University Health Sciences Center
El Paso, TX
Presenting Author(s)
Award: Presidential Poster Award
Andrew J. Ortega, DO, Sundar V. Cherukuri, DO, Mohammad Bashashati, MD, Irene Sarosiek, MD, Richard W. McCallum, MD, Sherif E. Elhanafi, MD
Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Gastroparesis (GP) is defined as delayed gastric emptying in the absence of mechanical obstruction. While medical therapies of GP are the first step. 30% or more of patients may require surgical or endoscopic interventions if GP is refractory to medications. EndoFLIP (Endoluminal Functional Lumen Imaging Probe) provides real-time measurements of cross-sectional area, pressure, and distensibility of various gastrointestinal (GI) sites. However, there have been limited applications to the pyloric sphincter (PS) where EndoFLIP could provide crucial investigative data to help determine the pathophysiological characteristics of the PS in refractory GP patients. Our study investigated (1) the effects of surgical pyloroplasty (PP) on EndoFLIP and gastric emptying (GE) outcomes and (2) whether there is PS pathology by comparing the number of interstitial cells of Cajal (ICC) between GP and control patients.
Methods: Eight patients with refractory GP (mean age: 50.5) failing medical therapies underwent laparoscopic robotic PP accompanied by gastric stimulator placement. Pyloric EndoFLIP was performed before and after PP at an inflated volume of 50mL of saline. A scintigraphic gastric emptying assessment was performed before and during follow-up to assess changes in GE. At surgery, pyloric biopsies were obtained from these refractory GP patients and compared to eight controls (non-GP autopsy specimens) regarding the number of ICC present per high power field (HPF). A T-test was used for the comparisons.
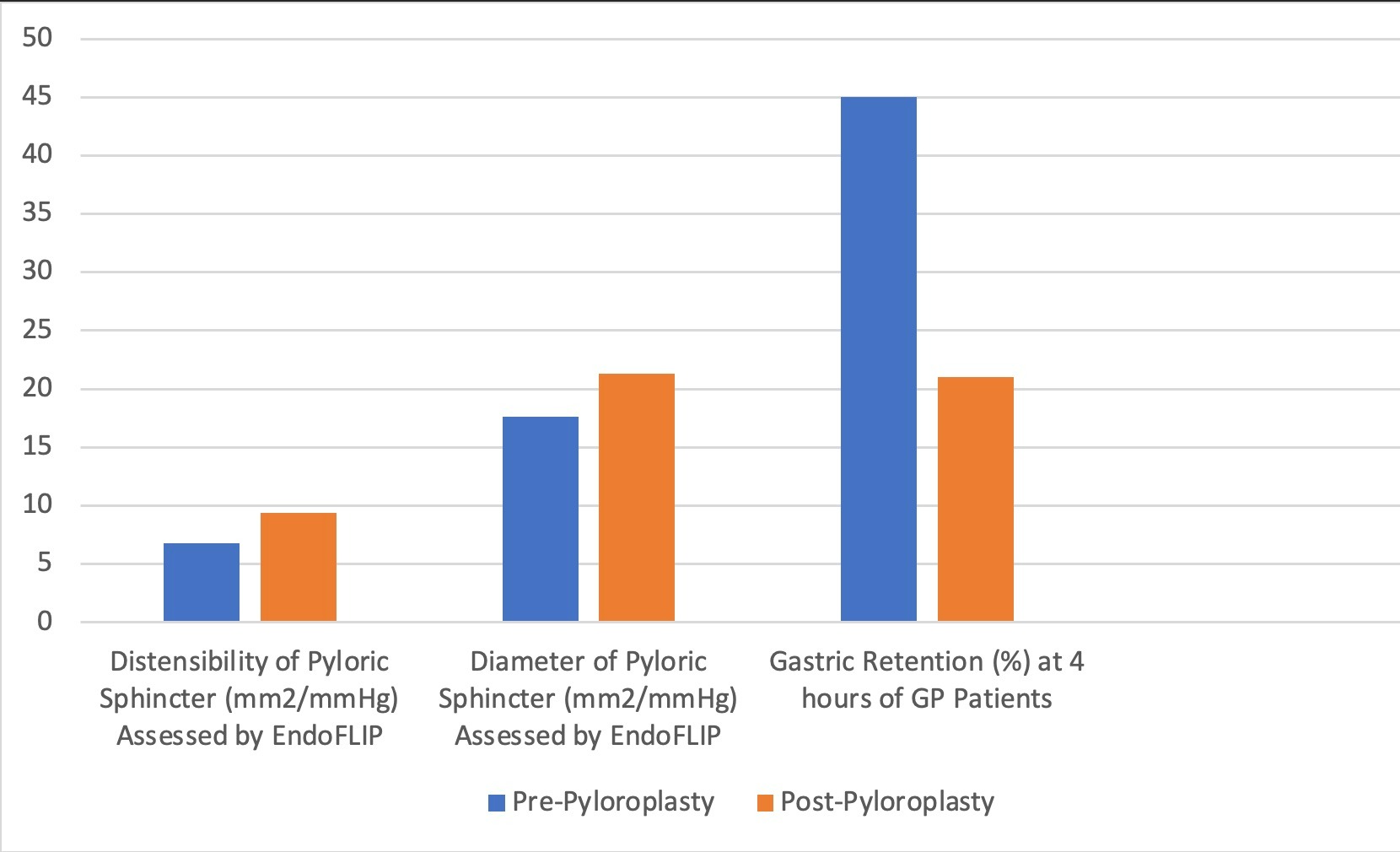
Results: Pre-PP pyloric distensibility and diameter at 50mL were 6.79 mm2/mmHg and 17.6 mm2/mmHg, respectively, with a mean pre-PP gastric retention of an isotope-labeled meal of 45% at 4 hours. Pyloric distensibility post-PP improved to 9.4 mm2/mmHg (p=0.28) with a significant pyloric diameter increase to 21.3 mm2/mmHg (p=0.05) (Figure 1). After PP, mean GE was 53% faster at 4 hours with gastric retention of 21% compared to the baseline. PS biopsy in GP patients had a mean ICC of 7.41 (SD: 2.3) per HPF, which was 36% lower than the ICC mean of 10.1 (SD:2.01) per HPF (p=0.09) present in the controls.
Discussion: 1) Pyloric EndoFLIP is an important new modality providing real-time data about the effectiveness of PP in medication refractory GP patients. 2) Our EndoFLIP findings indicate a significant improvement of diameter post-PP accompanied by a marked acceleration of GE. 3) There is pathology of the pyloric smooth muscle in GP as shown by a reduction in the number of ICC compared to controls.
Disclosures:
Andrew J. Ortega, DO, Sundar V. Cherukuri, DO, Mohammad Bashashati, MD, Irene Sarosiek, MD, Richard W. McCallum, MD, Sherif E. Elhanafi, MD. D0691 - Effects of Surgical Pyloroplasty on Pyloric EndoFLIP Measurements and Gastric Emptying in Patients With Refractory Gastroparesis and Identification of Pyloric Sphincter Smooth Muscle Pathology, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Andrew J. Ortega, DO, Sundar V. Cherukuri, DO, Mohammad Bashashati, MD, Irene Sarosiek, MD, Richard W. McCallum, MD, Sherif E. Elhanafi, MD
Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Gastroparesis (GP) is defined as delayed gastric emptying in the absence of mechanical obstruction. While medical therapies of GP are the first step. 30% or more of patients may require surgical or endoscopic interventions if GP is refractory to medications. EndoFLIP (Endoluminal Functional Lumen Imaging Probe) provides real-time measurements of cross-sectional area, pressure, and distensibility of various gastrointestinal (GI) sites. However, there have been limited applications to the pyloric sphincter (PS) where EndoFLIP could provide crucial investigative data to help determine the pathophysiological characteristics of the PS in refractory GP patients. Our study investigated (1) the effects of surgical pyloroplasty (PP) on EndoFLIP and gastric emptying (GE) outcomes and (2) whether there is PS pathology by comparing the number of interstitial cells of Cajal (ICC) between GP and control patients.
Methods: Eight patients with refractory GP (mean age: 50.5) failing medical therapies underwent laparoscopic robotic PP accompanied by gastric stimulator placement. Pyloric EndoFLIP was performed before and after PP at an inflated volume of 50mL of saline. A scintigraphic gastric emptying assessment was performed before and during follow-up to assess changes in GE. At surgery, pyloric biopsies were obtained from these refractory GP patients and compared to eight controls (non-GP autopsy specimens) regarding the number of ICC present per high power field (HPF). A T-test was used for the comparisons.
Results: Pre-PP pyloric distensibility and diameter at 50mL were 6.79 mm2/mmHg and 17.6 mm2/mmHg, respectively, with a mean pre-PP gastric retention of an isotope-labeled meal of 45% at 4 hours. Pyloric distensibility post-PP improved to 9.4 mm2/mmHg (p=0.28) with a significant pyloric diameter increase to 21.3 mm2/mmHg (p=0.05) (Figure 1). After PP, mean GE was 53% faster at 4 hours with gastric retention of 21% compared to the baseline. PS biopsy in GP patients had a mean ICC of 7.41 (SD: 2.3) per HPF, which was 36% lower than the ICC mean of 10.1 (SD:2.01) per HPF (p=0.09) present in the controls.
Discussion: 1) Pyloric EndoFLIP is an important new modality providing real-time data about the effectiveness of PP in medication refractory GP patients. 2) Our EndoFLIP findings indicate a significant improvement of diameter post-PP accompanied by a marked acceleration of GE. 3) There is pathology of the pyloric smooth muscle in GP as shown by a reduction in the number of ICC compared to controls.
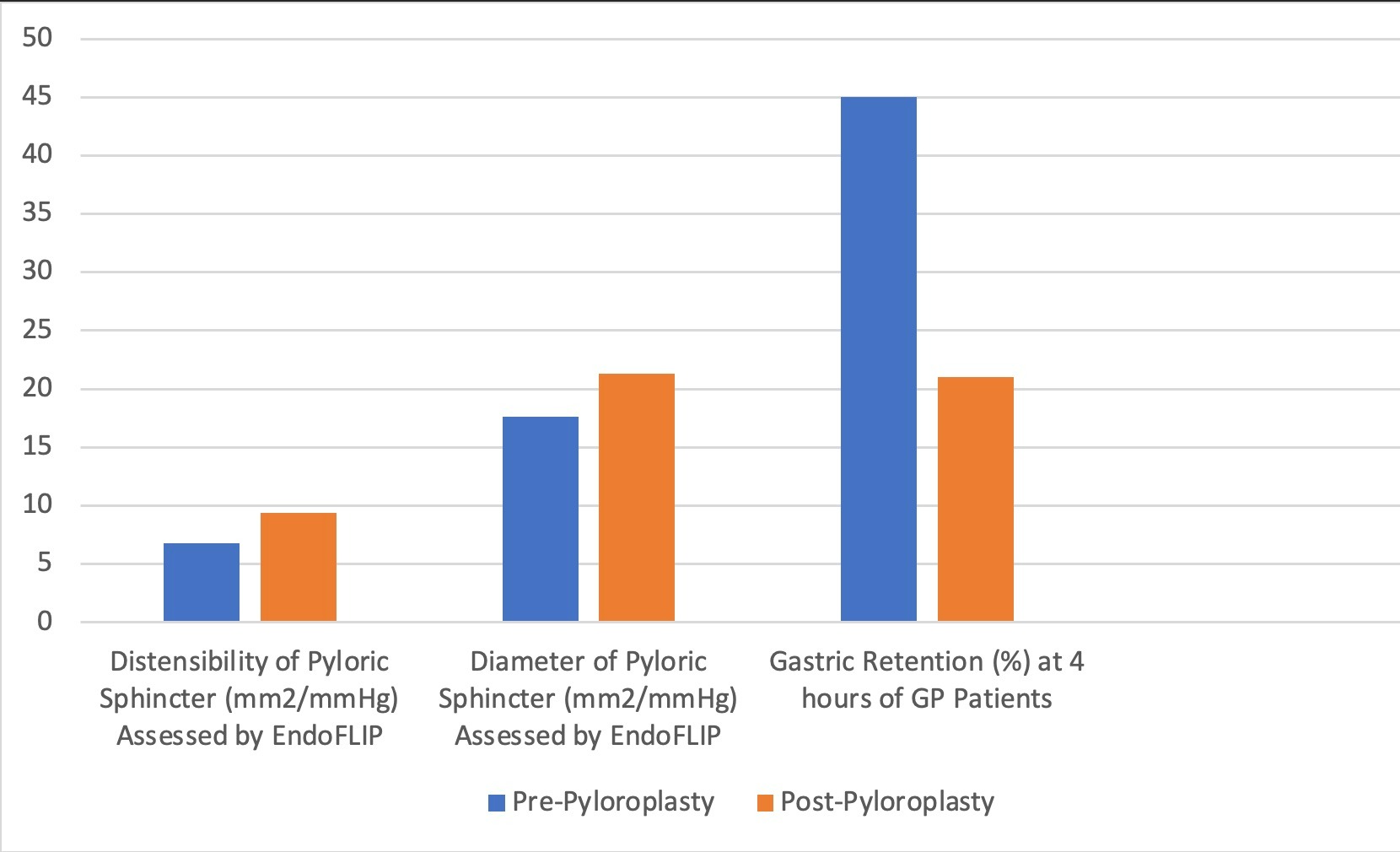
Figure: Figure 1: Measurements and comparisons of distensibility, diameter, and gastric retention pre and post-pyloroplasty using EndoFLIP
Disclosures:
Andrew Ortega indicated no relevant financial relationships.
Sundar Cherukuri indicated no relevant financial relationships.
Mohammad Bashashati indicated no relevant financial relationships.
Irene Sarosiek indicated no relevant financial relationships.
Richard McCallum indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Andrew J. Ortega, DO, Sundar V. Cherukuri, DO, Mohammad Bashashati, MD, Irene Sarosiek, MD, Richard W. McCallum, MD, Sherif E. Elhanafi, MD. D0691 - Effects of Surgical Pyloroplasty on Pyloric EndoFLIP Measurements and Gastric Emptying in Patients With Refractory Gastroparesis and Identification of Pyloric Sphincter Smooth Muscle Pathology, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

