Back


Poster Session C - Monday Afternoon
Category: Small Intestine
C0659 - A Deceptive Diagnosis: Gastric Outlet Obstruction in the Setting of Disseminated Tuberculosis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio
- RS
Radhika Sharma, DO
University of Florida College of Medicine
Jacksonville, FL
Presenting Author(s)
Radhika Sharma, DO, Abhinav Karan, MD, Shaorinkumar Patel, DO, Bruno D. Ribeiro, MD
University of Florida College of Medicine, Jacksonville, FL
Introduction: Tuberculosis (TB) continues to have a significant disease burden and while the most common manifestation of TB is pulmonary, primary abdominal tuberculosis is exceedingly rare. Duodenal involvement occurs in only about 0.3 to 2.3% of patients with TB. Even in parts of the world where TB is endemic, gastroduodenal tuberculosis accounts for only about 2% of disease burden. We present a rare case of a 52 year-old male who presented with primarily abdominal findings of constipation, epigastric pain, and intractable vomiting. The patient was initially mistaken to have lymphoma but diagnosed with gastric outlet obstruction secondary to disseminated tuberculosis.
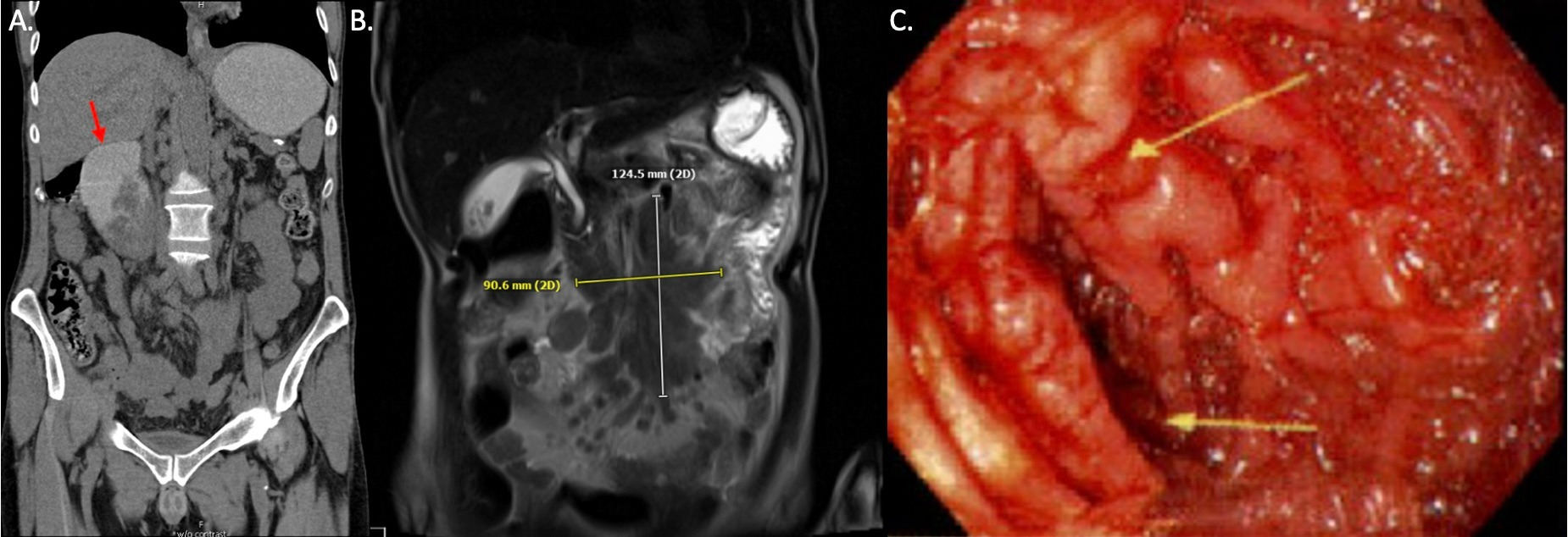
Case Description/Methods: A 52 year-old male with history of HIV presented to the ED with complaint of intractable non-bloody vomiting and severe epigastric abdominal pain. He reported a history of worsening constipation for which he had been seen in multiple EDs prior. On admission, the patient was found to have a lactic acidosis of 3.4 with severe abdominal distention and oral intolerance. A nasogastric tube was placed for gastric decompression. Computed tomography and magnetic resonance imaging revealed a conglomerate mesenteric nodal mass concerning for lymphoma. The mass was found to be compressing the horizontal segment of the duodenum resulting in a duodenal outlet obstruction.
Gastroenterology was consulted and performed an endoscopic ultrasound which revealed diffuse mucosal changes and moderate stenosis of the second portion of the duodenum. Enlarged celiac, peripancreatic, and porta hepatis lymph nodes were observed with appearance suggestive of lymphoma. Fine needle aspiration was positive for acid fast bacilli. Due to concerns for active pulmonary TB, the patient underwent bronchoscopy and bronchoalveolar lavage with cultures positive for acid fast bacilli and positive nucleic acid amplification (NAA) testing for Mycobacterium tuberculosis. The patient was started on RIPE therapy.
Discussion: Gastric outlet obstruction is an infrequently described presentation of TB. Our case highlights the importance of having a high index of suspicion for disseminated tuberculosis in an immunocompromised patient. Diagnosis requires either demonstration of caseating epithelioid granulomas or presence of acid-fast bacilli in tissue. GDTB is usually responsive to RIPE therapy. Surgical intervention is reserved for complications such as abscess, fistulas, or perforation.
Disclosures:
Radhika Sharma, DO, Abhinav Karan, MD, Shaorinkumar Patel, DO, Bruno D. Ribeiro, MD. C0659 - A Deceptive Diagnosis: Gastric Outlet Obstruction in the Setting of Disseminated Tuberculosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Florida College of Medicine, Jacksonville, FL
Introduction: Tuberculosis (TB) continues to have a significant disease burden and while the most common manifestation of TB is pulmonary, primary abdominal tuberculosis is exceedingly rare. Duodenal involvement occurs in only about 0.3 to 2.3% of patients with TB. Even in parts of the world where TB is endemic, gastroduodenal tuberculosis accounts for only about 2% of disease burden. We present a rare case of a 52 year-old male who presented with primarily abdominal findings of constipation, epigastric pain, and intractable vomiting. The patient was initially mistaken to have lymphoma but diagnosed with gastric outlet obstruction secondary to disseminated tuberculosis.
Case Description/Methods: A 52 year-old male with history of HIV presented to the ED with complaint of intractable non-bloody vomiting and severe epigastric abdominal pain. He reported a history of worsening constipation for which he had been seen in multiple EDs prior. On admission, the patient was found to have a lactic acidosis of 3.4 with severe abdominal distention and oral intolerance. A nasogastric tube was placed for gastric decompression. Computed tomography and magnetic resonance imaging revealed a conglomerate mesenteric nodal mass concerning for lymphoma. The mass was found to be compressing the horizontal segment of the duodenum resulting in a duodenal outlet obstruction.
Gastroenterology was consulted and performed an endoscopic ultrasound which revealed diffuse mucosal changes and moderate stenosis of the second portion of the duodenum. Enlarged celiac, peripancreatic, and porta hepatis lymph nodes were observed with appearance suggestive of lymphoma. Fine needle aspiration was positive for acid fast bacilli. Due to concerns for active pulmonary TB, the patient underwent bronchoscopy and bronchoalveolar lavage with cultures positive for acid fast bacilli and positive nucleic acid amplification (NAA) testing for Mycobacterium tuberculosis. The patient was started on RIPE therapy.
Discussion: Gastric outlet obstruction is an infrequently described presentation of TB. Our case highlights the importance of having a high index of suspicion for disseminated tuberculosis in an immunocompromised patient. Diagnosis requires either demonstration of caseating epithelioid granulomas or presence of acid-fast bacilli in tissue. GDTB is usually responsive to RIPE therapy. Surgical intervention is reserved for complications such as abscess, fistulas, or perforation.
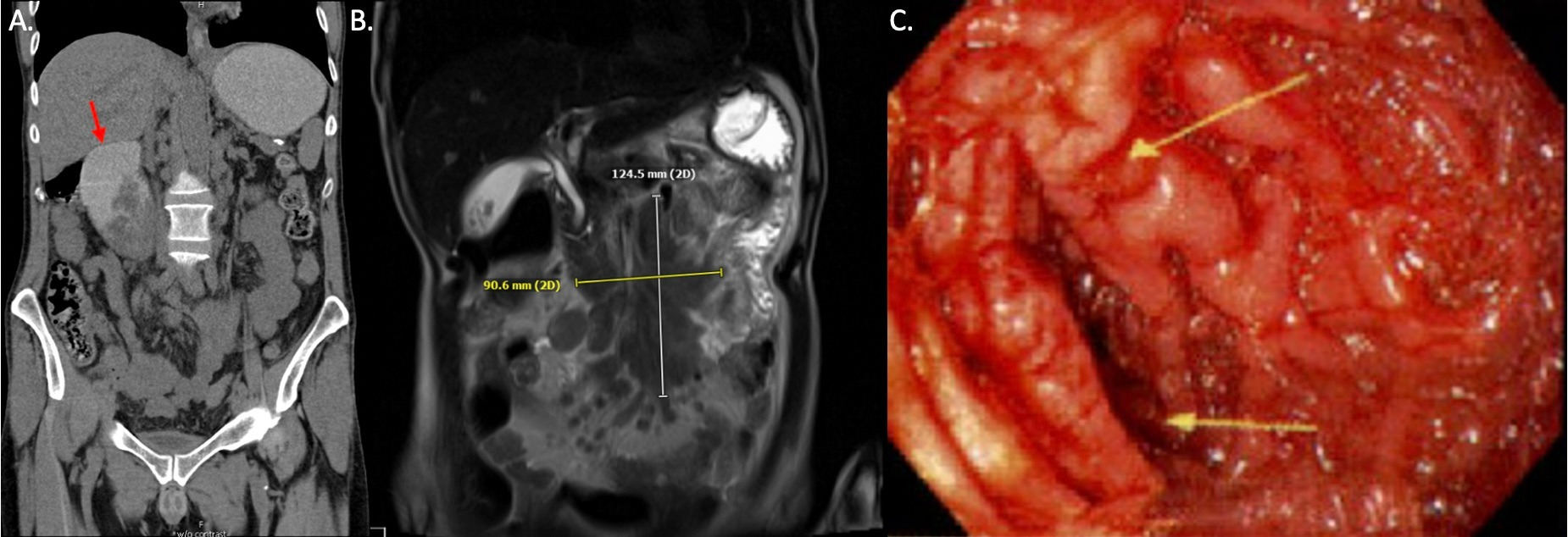
Figure: Figure 1 (A) Computed tomography and (B) Magnetic resonance imaging revealed a conglomerate mesenteric nodal mass concerning for lymphoma. The mass was found to be compressing the horizontal segment of the duodenum resulting in a duodenal outlet obstruction. (C) EGD revealed diffuse mucosal changes and moderate stenosis of the second portion of the duodenum.
Disclosures:
Radhika Sharma indicated no relevant financial relationships.
Abhinav Karan indicated no relevant financial relationships.
Shaorinkumar Patel indicated no relevant financial relationships.
Bruno Ribeiro indicated no relevant financial relationships.
Radhika Sharma, DO, Abhinav Karan, MD, Shaorinkumar Patel, DO, Bruno D. Ribeiro, MD. C0659 - A Deceptive Diagnosis: Gastric Outlet Obstruction in the Setting of Disseminated Tuberculosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
