Back

Poster Session D - Tuesday Morning
Category: Stomach
D0733 - Gastric Crohn's Disease
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Syed Salman Hamid Hashmi, MD
NYU Langone Medical Center/ Woodhull Medical Center
New York, New York
Presenting Author(s)
Syed Salman Hamid Hashmi, MD1, Rohit Gupta, DO2, Ahmed Shady, MD3, Yvette Achuo-Egbe, MD, MPH, MS4, Gulam Mustafa Khan, MD1, Graham Mason, MD1
1NYU Langone Medical Center/ Woodhull Medical Center, New York, NY; 2New York Medical Center/ Metropolitan Hospital, New York, NY; 3New York Medical College/ Metropolitan Medical Center, New York, NY; 4New York Medical College/ NYCHH- Metropolitan Hospital Center, New York, NY
Introduction: Crohn’s disease is an idiopathic transmural, segmental inflammatory disease of the gastrointestinal tract mostly involving the small intestine, colon, and anorectal region. We report a very rare case of isolated gastric Crohn's disease (GCD).
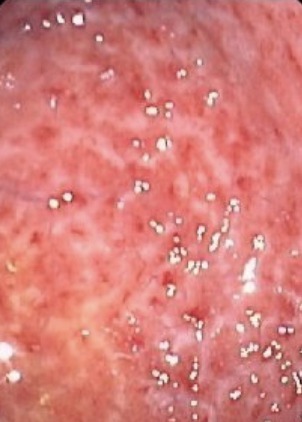
Case Description/Methods: A 26-year-old African- American male was referred to the outpatient gastroenterology clinic for a complaint of worsening dyspepsia, nausea, and vomiting for a year. The patient received a 16-week course of pantoprazole with partial relief. The preliminary laboratory workup for the patient was negative. The upper endoscopy of the patient revealed gastritis in the antrum of the stomach and a biopsy revealed non-caseating granuloma with giant cells. Helicobacter pylori test was negative and the serological test was negative for anti-saccharomyces cerevisiae antibody. The chest X-ray of the patient was normal. A barium follow-through and a colonoscopy of the patient were normal. After ruling out other causes of granulomatous gastritis a diagnosis of isolated gastric Crohn’s disease was made. The patient was started on oral steroids and his dyspepsia completely resolved in the 3 months follow-up. A repeat endoscopy after 6 months revealed resolution of gastritis and a biopsy revealed no granulomas. The diagnosis of Crohn's disease in typical presentations is made based on a combination of clinical, laboratory, endoscopic and pathological findings. In our case, the patient had an atypical presentation and ASCA was negative. In such cases, other possible etiologies like Helicobacter pylori infection, tuberculosis, eosinophilic gastritis, sarcoidosis, and lymphoma must be ruled out for establishing the diagnosis.
Discussion: Patients with GCD generally present with epigastric pain, nausea, and vomiting and an upper endoscopy generally shows diffuse inflammation and granular lesions. It is important to keep GCD as a differential diagnosis for young patients who present with dyspepsia-like symptoms and don't respond to proton pump therapy.
Disclosures:
Syed Salman Hamid Hashmi, MD1, Rohit Gupta, DO2, Ahmed Shady, MD3, Yvette Achuo-Egbe, MD, MPH, MS4, Gulam Mustafa Khan, MD1, Graham Mason, MD1. D0733 - Gastric Crohn's Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1NYU Langone Medical Center/ Woodhull Medical Center, New York, NY; 2New York Medical Center/ Metropolitan Hospital, New York, NY; 3New York Medical College/ Metropolitan Medical Center, New York, NY; 4New York Medical College/ NYCHH- Metropolitan Hospital Center, New York, NY
Introduction: Crohn’s disease is an idiopathic transmural, segmental inflammatory disease of the gastrointestinal tract mostly involving the small intestine, colon, and anorectal region. We report a very rare case of isolated gastric Crohn's disease (GCD).
Case Description/Methods: A 26-year-old African- American male was referred to the outpatient gastroenterology clinic for a complaint of worsening dyspepsia, nausea, and vomiting for a year. The patient received a 16-week course of pantoprazole with partial relief. The preliminary laboratory workup for the patient was negative. The upper endoscopy of the patient revealed gastritis in the antrum of the stomach and a biopsy revealed non-caseating granuloma with giant cells. Helicobacter pylori test was negative and the serological test was negative for anti-saccharomyces cerevisiae antibody. The chest X-ray of the patient was normal. A barium follow-through and a colonoscopy of the patient were normal. After ruling out other causes of granulomatous gastritis a diagnosis of isolated gastric Crohn’s disease was made. The patient was started on oral steroids and his dyspepsia completely resolved in the 3 months follow-up. A repeat endoscopy after 6 months revealed resolution of gastritis and a biopsy revealed no granulomas. The diagnosis of Crohn's disease in typical presentations is made based on a combination of clinical, laboratory, endoscopic and pathological findings. In our case, the patient had an atypical presentation and ASCA was negative. In such cases, other possible etiologies like Helicobacter pylori infection, tuberculosis, eosinophilic gastritis, sarcoidosis, and lymphoma must be ruled out for establishing the diagnosis.
Discussion: Patients with GCD generally present with epigastric pain, nausea, and vomiting and an upper endoscopy generally shows diffuse inflammation and granular lesions. It is important to keep GCD as a differential diagnosis for young patients who present with dyspepsia-like symptoms and don't respond to proton pump therapy.
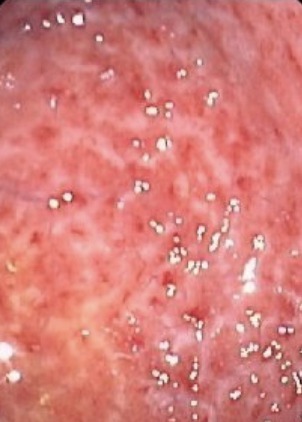
Figure: The image shows granulomatous gastritis on the upper endoscopy.
Disclosures:
Syed Salman Hamid Hashmi indicated no relevant financial relationships.
Rohit Gupta indicated no relevant financial relationships.
Ahmed Shady indicated no relevant financial relationships.
Yvette Achuo-Egbe indicated no relevant financial relationships.
Gulam Mustafa Khan indicated no relevant financial relationships.
Graham Mason indicated no relevant financial relationships.
Syed Salman Hamid Hashmi, MD1, Rohit Gupta, DO2, Ahmed Shady, MD3, Yvette Achuo-Egbe, MD, MPH, MS4, Gulam Mustafa Khan, MD1, Graham Mason, MD1. D0733 - Gastric Crohn's Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
