Back

Poster Session B - Monday Morning
Category: Liver
B0540 - A Rare Epstein-Barr Virus-Associated Tumor of the Liver and Spleen
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- SB
Shoma Bommena, MD
Banner University Medical Center, University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Shoma Bommena, MD1, Rohit Nathan, DO2
1Banner University Medical Center, University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona College of Medicine, Phoenix, AZ
Introduction: Inflammatory Pseudotumor-like follicular dendritic cell tumor (IPT-like FDC) is a rare histological subtype of follicle dendritic cell tumors, with unique clinical and pathological characteristics characterized by an intense lymphoplasmacytic infiltrate mixed with a neoplastic spindle, and consistent association with Epstein-Barr virus (EBV). We describe a rare case of splenic ITP-like FDC with hepatic metastasis.
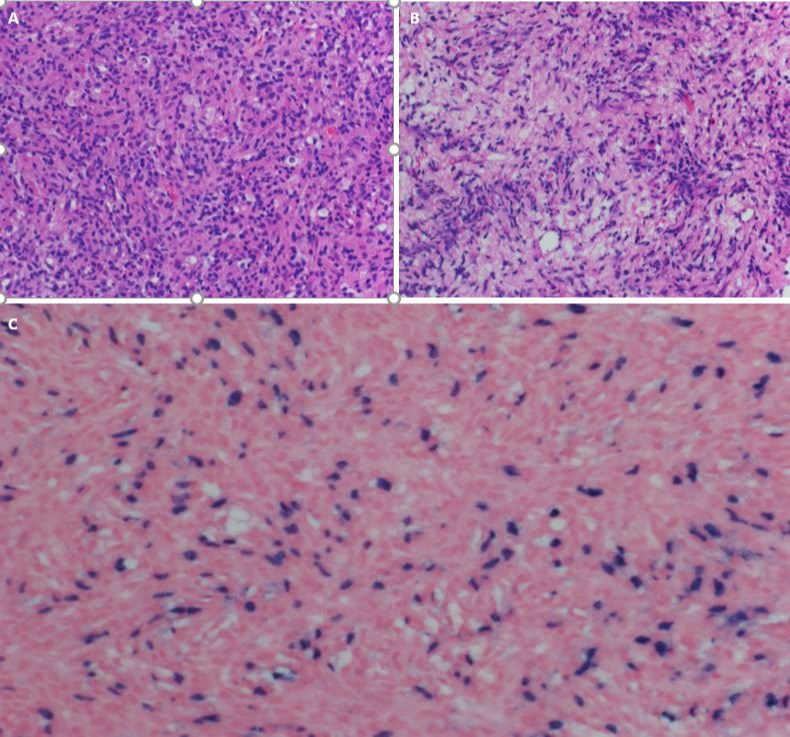
Case Description/Methods: A 67-year-old female with unremarkable medical history presented with a one-day history of periumbilical abdominal pain and was found to have incidental findings of hypodense hepatic and splenic lesions on abdominal CT. Subsequent MRI abdomen showed numerous new peripherally enhancing hypodense lesions throughout the liver and a slightly enlarged 8.0 x 5.5 cm heterogeneously enhancing splenic lesion, seen in scans dated ten years back. These radiological findings, combined with histological evidence of an atypical EBV-associated lymphohistiocytic proliferation obtained from a biopsy of the hypoechoic liver mass (Figure), helped diagnose IPT-like FDC that started in the spleen and later metastasized to the liver. Surgical resection with Right hepatectomy, wedge resection of the left-sided lesion, and splenectomy was recommended to reduce the tumor burden. Unfortunately, the patient did not follow up and pursue surgical options due to the pandemic. Repeat imaging two years later showed multiple enhancing liver lesions and enlarged splenic lesions. Given the progression of the disease, surgical resection was not an option, and the medical oncology team initiated systemic treatment with Gemcitabine and Docetaxel. Imaging after four months showed a slightly decreased size of metastatic hepatic disease and dominant splenic mass.
Discussion: IPT-like FDC accounts for less than 1% of all primary splenic and hepatic tumors, with female predominance. It should be differentiated from classic FDC, IPT, and Inflammatory myofibroblastic tumors by examining morphological features combined with immunohistochemistry, including FDC markers: CD21, CD35, and CD23, clustering, CNA.42, CXCL-13, and D2.40 (podoplanin). Detection of EBV-encoded RNA by in situ hybridization supports the diagnosis. Given the indolent clinical course with low malignant potential, Surgical resection is the mainstay of treatment for localized lesions, with systemic chemotherapy and radiation therapy used in nonoperative cases, but efficacy is unclear.
Disclosures:
Shoma Bommena, MD1, Rohit Nathan, DO2. B0540 - A Rare Epstein-Barr Virus-Associated Tumor of the Liver and Spleen, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Banner University Medical Center, University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona College of Medicine, Phoenix, AZ
Introduction: Inflammatory Pseudotumor-like follicular dendritic cell tumor (IPT-like FDC) is a rare histological subtype of follicle dendritic cell tumors, with unique clinical and pathological characteristics characterized by an intense lymphoplasmacytic infiltrate mixed with a neoplastic spindle, and consistent association with Epstein-Barr virus (EBV). We describe a rare case of splenic ITP-like FDC with hepatic metastasis.
Case Description/Methods: A 67-year-old female with unremarkable medical history presented with a one-day history of periumbilical abdominal pain and was found to have incidental findings of hypodense hepatic and splenic lesions on abdominal CT. Subsequent MRI abdomen showed numerous new peripherally enhancing hypodense lesions throughout the liver and a slightly enlarged 8.0 x 5.5 cm heterogeneously enhancing splenic lesion, seen in scans dated ten years back. These radiological findings, combined with histological evidence of an atypical EBV-associated lymphohistiocytic proliferation obtained from a biopsy of the hypoechoic liver mass (Figure), helped diagnose IPT-like FDC that started in the spleen and later metastasized to the liver. Surgical resection with Right hepatectomy, wedge resection of the left-sided lesion, and splenectomy was recommended to reduce the tumor burden. Unfortunately, the patient did not follow up and pursue surgical options due to the pandemic. Repeat imaging two years later showed multiple enhancing liver lesions and enlarged splenic lesions. Given the progression of the disease, surgical resection was not an option, and the medical oncology team initiated systemic treatment with Gemcitabine and Docetaxel. Imaging after four months showed a slightly decreased size of metastatic hepatic disease and dominant splenic mass.
Discussion: IPT-like FDC accounts for less than 1% of all primary splenic and hepatic tumors, with female predominance. It should be differentiated from classic FDC, IPT, and Inflammatory myofibroblastic tumors by examining morphological features combined with immunohistochemistry, including FDC markers: CD21, CD35, and CD23, clustering, CNA.42, CXCL-13, and D2.40 (podoplanin). Detection of EBV-encoded RNA by in situ hybridization supports the diagnosis. Given the indolent clinical course with low malignant potential, Surgical resection is the mainstay of treatment for localized lesions, with systemic chemotherapy and radiation therapy used in nonoperative cases, but efficacy is unclear.
Figure: Figure: Dense lymphohistiocytic and spindle cell infiltrate in the liver (hematoxylin-eosin stain, panel A & B). EBER (EBV encoded RNA) in situ hybridization shows positive staining of many neoplastic cells (panel C).
Disclosures:
Shoma Bommena indicated no relevant financial relationships.
Rohit Nathan indicated no relevant financial relationships.
Shoma Bommena, MD1, Rohit Nathan, DO2. B0540 - A Rare Epstein-Barr Virus-Associated Tumor of the Liver and Spleen, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
