Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0222 - A Rare Case of Acute Esophageal Necrosis Precipitated by Klebsiella pneumoniae
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Lekha Yadukumar, MD
The Wright Center for GME
Scranton, PA
Presenting Author(s)
Lekha Yadukumar, MD, Hunain Aslam, MD, Khalid Ahmed, MD, Omar Syed, MD, Khadijah Sajid, MD
The Wright Center for GME, Scranton, PA
Introduction: Acute esophageal necrosis (AEN) is a rare ischemic condition diagnosed on endoscopy (EGD) by black appearance of the esophagus. Its pathophysiology is multifactorial and often associated with underlying comorbidities such as age, malnourishment, ischemia and debilitated state. Early identification, appropriate management are associated with better outcomes. Treatment is primarily conservative therapy. In our case report we will discuss a patient who was found to have AEN in the presence of Klebsiella pneumonia.
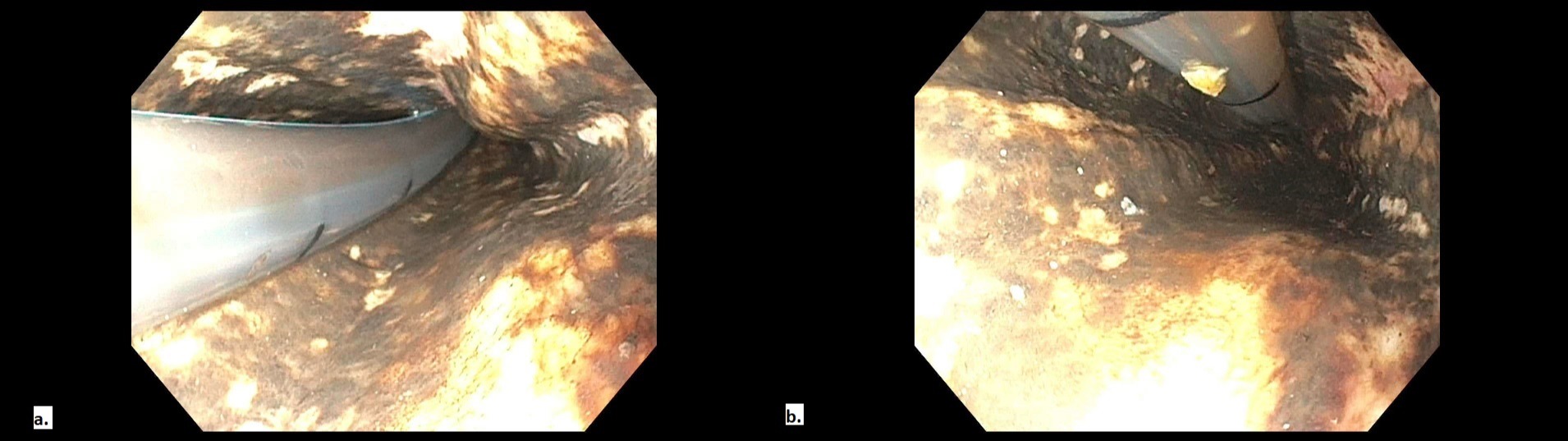
Case Description/Methods: 88-year-old active male with no significant medical history presented to the ED with syncope and neck pain. He was tachycardic, found to have bilateral cervical C6 spine fracture and epidural hematoma at the level of C2-C3 with posterior CSF leak on imaging. Xray showed airspace opacities in the left lower lobe. Shortly afterwards he developed hyponatremia, altered mental status and coffee ground emesis. He underwent emergent EGD with biopsy which revealed multiple plaques in the proximal esophagus 25 cm from the gastroesophageal junction with circumferential “black esophagus” (figure 1). Biopsy revealed necrotic esophageal squamous mucosa with associated acute inflammation and necrotic debri. He was started on pantoprazole and fluid infusion. Bronchial aspirate was positive for Klebsiella pneumoniae and he was treated with ceftriaxone. He was found to have worsening posterior epidural hematoma with severe spinal cord and canal compression and underwent emergent laminectomy however his condition continued to deteriorate and he eventually passed away.
Discussion: AEN must be considered as a cause of upper gastrointestinal bleeding especially in patients with the risk factors of advanced vasculopathy including male gender, advanced age, diabetes mellitus, dyslipidemia and ischemic cardiomyopathy and a debilitated physical state consisting of malnutrition and/or recent history of malignancy. The pathophysiology is likely due to hypoperfusion, followed by weakened protective barrier and gastric reflux. If there is any underlying infection, there is a high possibility of dissemination of the infection to precipitate AEN. Hence, it must be recognized early, with aggressive management to improve clinical outcomes. Management entails treating the underlying pathology, early PPI infusion and maintaining hydration. NG tube should be avoided due to risk of perforation and surgical intervention are reserved for complex AEN or complications.
Disclosures:
Lekha Yadukumar, MD, Hunain Aslam, MD, Khalid Ahmed, MD, Omar Syed, MD, Khadijah Sajid, MD. D0222 - A Rare Case of Acute Esophageal Necrosis Precipitated by Klebsiella pneumoniae, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
The Wright Center for GME, Scranton, PA
Introduction: Acute esophageal necrosis (AEN) is a rare ischemic condition diagnosed on endoscopy (EGD) by black appearance of the esophagus. Its pathophysiology is multifactorial and often associated with underlying comorbidities such as age, malnourishment, ischemia and debilitated state. Early identification, appropriate management are associated with better outcomes. Treatment is primarily conservative therapy. In our case report we will discuss a patient who was found to have AEN in the presence of Klebsiella pneumonia.
Case Description/Methods: 88-year-old active male with no significant medical history presented to the ED with syncope and neck pain. He was tachycardic, found to have bilateral cervical C6 spine fracture and epidural hematoma at the level of C2-C3 with posterior CSF leak on imaging. Xray showed airspace opacities in the left lower lobe. Shortly afterwards he developed hyponatremia, altered mental status and coffee ground emesis. He underwent emergent EGD with biopsy which revealed multiple plaques in the proximal esophagus 25 cm from the gastroesophageal junction with circumferential “black esophagus” (figure 1). Biopsy revealed necrotic esophageal squamous mucosa with associated acute inflammation and necrotic debri. He was started on pantoprazole and fluid infusion. Bronchial aspirate was positive for Klebsiella pneumoniae and he was treated with ceftriaxone. He was found to have worsening posterior epidural hematoma with severe spinal cord and canal compression and underwent emergent laminectomy however his condition continued to deteriorate and he eventually passed away.
Discussion: AEN must be considered as a cause of upper gastrointestinal bleeding especially in patients with the risk factors of advanced vasculopathy including male gender, advanced age, diabetes mellitus, dyslipidemia and ischemic cardiomyopathy and a debilitated physical state consisting of malnutrition and/or recent history of malignancy. The pathophysiology is likely due to hypoperfusion, followed by weakened protective barrier and gastric reflux. If there is any underlying infection, there is a high possibility of dissemination of the infection to precipitate AEN. Hence, it must be recognized early, with aggressive management to improve clinical outcomes. Management entails treating the underlying pathology, early PPI infusion and maintaining hydration. NG tube should be avoided due to risk of perforation and surgical intervention are reserved for complex AEN or complications.
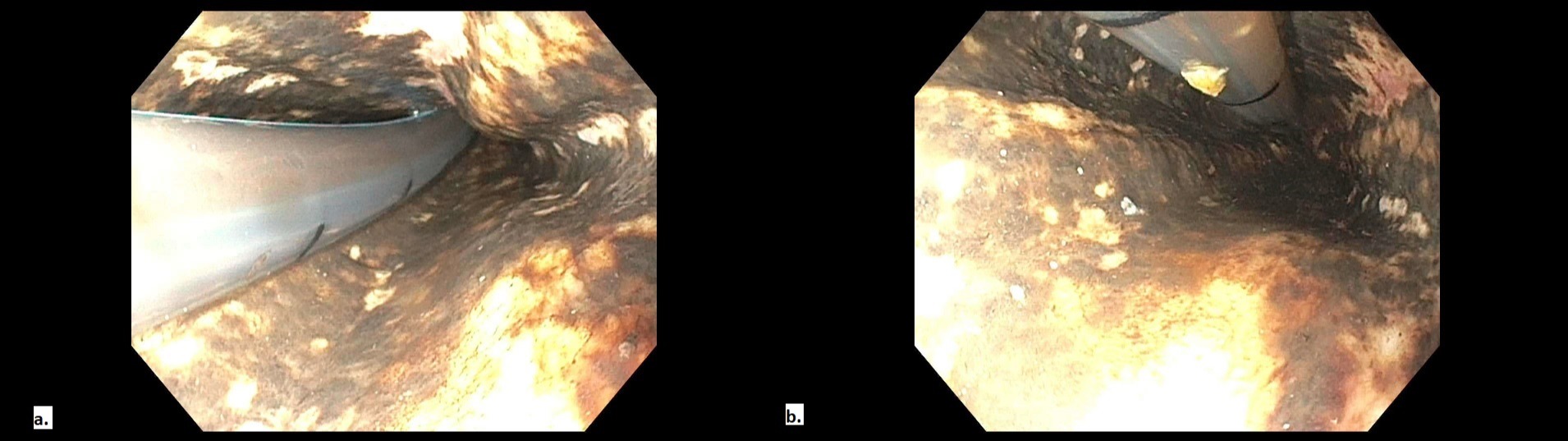
Figure: Endoscopy images of lower third (a) and middle third (b) of the esophagus showing " black esophagus"
Disclosures:
Lekha Yadukumar indicated no relevant financial relationships.
Hunain Aslam indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Omar Syed indicated no relevant financial relationships.
Khadijah Sajid indicated no relevant financial relationships.
Lekha Yadukumar, MD, Hunain Aslam, MD, Khalid Ahmed, MD, Omar Syed, MD, Khadijah Sajid, MD. D0222 - A Rare Case of Acute Esophageal Necrosis Precipitated by Klebsiella pneumoniae, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
