Back

Poster Session A - Sunday Afternoon
Category: Liver
A0522 - A Case of Liver Failure Secondary to Chronic Intestinal Failure and Augmentin Use
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Anita Mahadevan, BA
Case Western Reserve University School of Medicine
Cleveland, OH
Presenting Author(s)
Anita Mahadevan, BA1, Bianca Islam, MD, PhD2, Naemat Sandhu, 3
1Case Western Reserve University School of Medicine, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospital, Cleveland, OH
Introduction: We present a case of acute on chronic liver failure in a patient on chronic Augmentin and total parenteral nutrition (TPN). We highlight the mechanisms and key findings of liver injury associated with intestinal failure and Augmentin, which are relevant for evaluating the risks and benefits of such therapies.
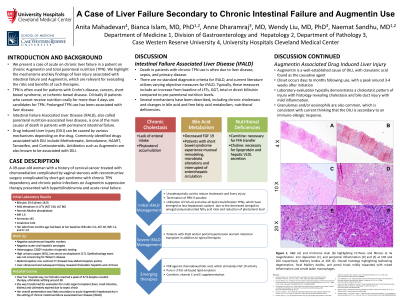
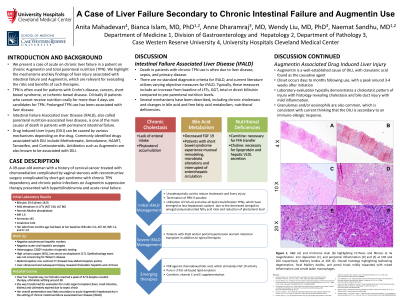
Case Description/Methods: A 49-year-old woman with a history of cervical cancer treated with chemoradiation complicated by vaginal stenosis with reconstructive surgery complicated by short gut syndrome with chronic TPN dependency and chronic pelvic infections on Augmentin suppression therapy presented with hyperbilirubinemia and acute renal failure. Initial laboratory results include bilirubin 29.4 (predominantly direct), mildly elevated liver enzymes, normal alkaline phosphatase, INR 1.6, and creatinine 3.64. Her TPN and Augmentin were held. Evaluation for autoimmune markers and acute viral hepatitis serologies were negative. Genetic testing showed heterozygous C282Y mutation. Urinary copper was high with low serum ceruloplasmin, however ophthalmology exam was not concerning for Wilson’s disease. Abdominopelvic non-contrast CT showed new abdominopelvic ascites. Liver biopsy revealed cholestatic hepatitis and cirrhosis. Her presentation was likely secondary to acute Augmentin hepatotoxicity in the setting of chronic intestinal-failure associated liver disease (IFALD). The patient ultimately expired due to septic shock.
Discussion: Augmentin is a known cause of DILI, with clavulanic acid established as the causative agent. Onset occurs days to months following use and liver histology reveals cholestasis, bile duct inflammation and commonly granulomas and eosinophils, which is consistent with current thinking that the DILI is an immunoallergic response.
IFALD has a multifactorial disease process. Chronic cholestasis has been shown to occur in TPN-dependent patients, due to lack of enteral intake stimulating bile flow and hepatocyte phytosterol accumulation interfering with bile acid secretion in patients utilizing soybean-oil lipid emulsions. Steatosis has been linked to TPN-induced depletion of carnitine and choline, which results in disrupted hepatocyte lipid transport and storage. Liver histology reveals cholestasis, portal inflammation, macrosteatosis, and ductular proliferation. TPN formulas with fish-oil and olive-oil lipid emulsions are emerging as less hepatotoxic. Ursodiol may reduce cholestasis and liver injury. Death is often due to liver disease, sepsis, and primary disease.
Disclosures:
Anita Mahadevan, BA1, Bianca Islam, MD, PhD2, Naemat Sandhu, 3. A0522 - A Case of Liver Failure Secondary to Chronic Intestinal Failure and Augmentin Use, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Case Western Reserve University School of Medicine, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospital, Cleveland, OH
Introduction: We present a case of acute on chronic liver failure in a patient on chronic Augmentin and total parenteral nutrition (TPN). We highlight the mechanisms and key findings of liver injury associated with intestinal failure and Augmentin, which are relevant for evaluating the risks and benefits of such therapies.
Case Description/Methods: A 49-year-old woman with a history of cervical cancer treated with chemoradiation complicated by vaginal stenosis with reconstructive surgery complicated by short gut syndrome with chronic TPN dependency and chronic pelvic infections on Augmentin suppression therapy presented with hyperbilirubinemia and acute renal failure. Initial laboratory results include bilirubin 29.4 (predominantly direct), mildly elevated liver enzymes, normal alkaline phosphatase, INR 1.6, and creatinine 3.64. Her TPN and Augmentin were held. Evaluation for autoimmune markers and acute viral hepatitis serologies were negative. Genetic testing showed heterozygous C282Y mutation. Urinary copper was high with low serum ceruloplasmin, however ophthalmology exam was not concerning for Wilson’s disease. Abdominopelvic non-contrast CT showed new abdominopelvic ascites. Liver biopsy revealed cholestatic hepatitis and cirrhosis. Her presentation was likely secondary to acute Augmentin hepatotoxicity in the setting of chronic intestinal-failure associated liver disease (IFALD). The patient ultimately expired due to septic shock.
Discussion: Augmentin is a known cause of DILI, with clavulanic acid established as the causative agent. Onset occurs days to months following use and liver histology reveals cholestasis, bile duct inflammation and commonly granulomas and eosinophils, which is consistent with current thinking that the DILI is an immunoallergic response.
IFALD has a multifactorial disease process. Chronic cholestasis has been shown to occur in TPN-dependent patients, due to lack of enteral intake stimulating bile flow and hepatocyte phytosterol accumulation interfering with bile acid secretion in patients utilizing soybean-oil lipid emulsions. Steatosis has been linked to TPN-induced depletion of carnitine and choline, which results in disrupted hepatocyte lipid transport and storage. Liver histology reveals cholestasis, portal inflammation, macrosteatosis, and ductular proliferation. TPN formulas with fish-oil and olive-oil lipid emulsions are emerging as less hepatotoxic. Ursodiol may reduce cholestasis and liver injury. Death is often due to liver disease, sepsis, and primary disease.
Disclosures:
Anita Mahadevan indicated no relevant financial relationships.
Bianca Islam indicated no relevant financial relationships.
Naemat Sandhu indicated no relevant financial relationships.
Anita Mahadevan, BA1, Bianca Islam, MD, PhD2, Naemat Sandhu, 3. A0522 - A Case of Liver Failure Secondary to Chronic Intestinal Failure and Augmentin Use, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

