Back
Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0062 - Diffuse Large B Cell Lymphoma Presenting as Acute Recurrent Pancreatitis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Shalini S. Jain, MD
CHI Creighton University Medical Center
Omaha, NE
Presenting Author(s)
Shalini S. Jain, MD1, Faith Abodunrin, MD1, Michael McCabe, MD2
1CHI Creighton University Medical Center, Omaha, NE; 2Rocky Mountain Gastroenterology Association, Lakewood, CO
Introduction: Extra-nodal Non-Hodgkin’s lymphomas are mostly made of gastrointestinal sites1. Primary pancreatic lymphomas account for < 1% of all extra-nodal lymphomas and are extremely rare. Diagnosis is often missed or delayed due to the prevalence of chronic pancreatitis or pancreatic adenocarcinoma as thought to be the main causes of any pancreatic stricture or mass seen when diagnosing a patient. We present a case of pancreatic lymphoma presenting as acute recurrent pancreatitis.
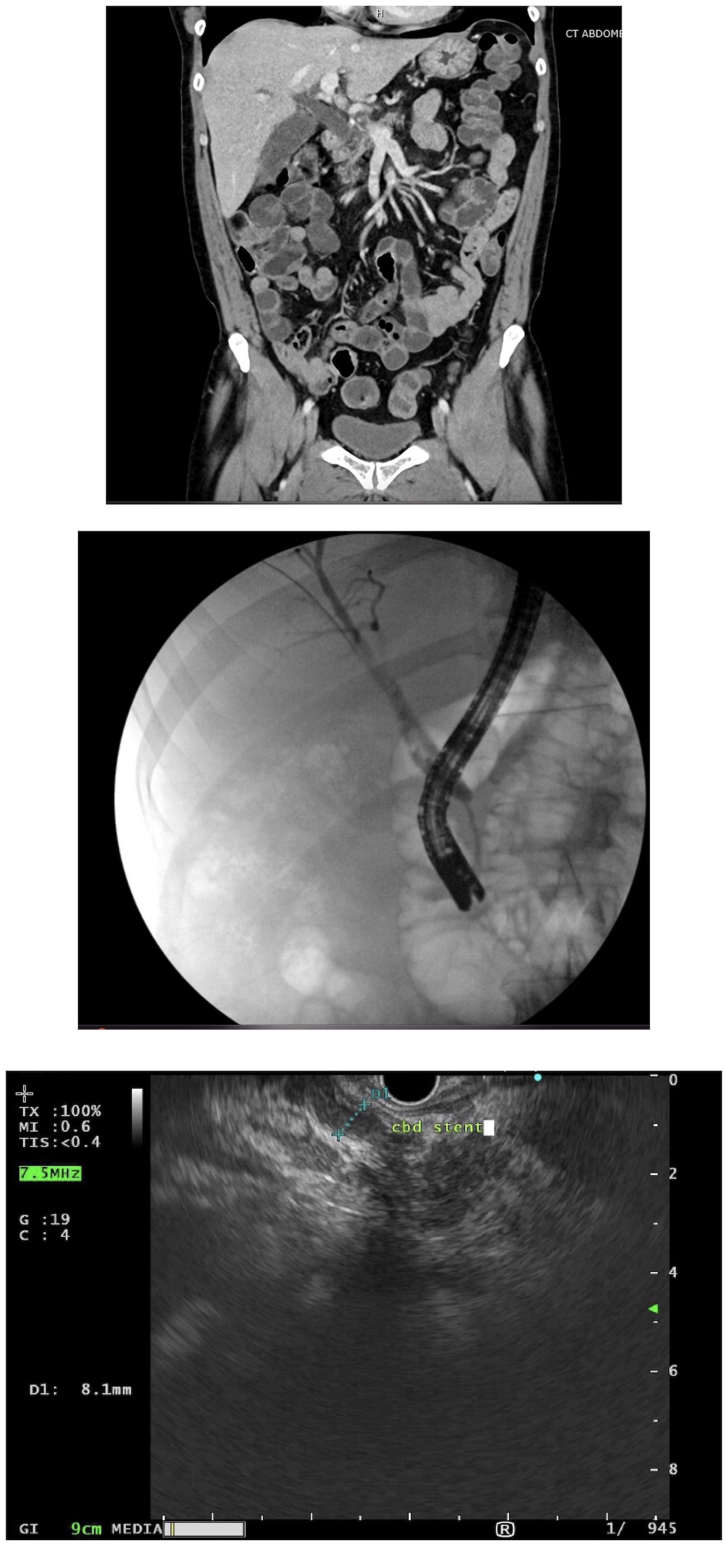
Case Description/Methods: A 51-year-old male with past medical history of rheumatoid arthritis and nicotine use presented with jaundice, abdominal pain, and fatigue and 30-pound weight loss. MRCP showed intra- and extra-hepatic biliary dilation, showing double duct sign. CT suggested acute pancreatitis. ERCP was done showing a single localized biliary malignant appearing stricture in the lower third of the main bile duct with upstream dilation. EUS showed a 19 mm by 19 mm mass in the head of pancreas and 8 mm dilation of the common bile duct. EUS fine needle biopsy showed chronic pancreatitis with dense fibrosis and benign peri-pancreatic lymph nodes. PET CT showed activity in the pancreas and retroperitoneal lymph nodes. Tumor markers (AFP, CEA, CA 19-9) were within normal limits. Patient had no known risk factors for chronic pancreatitis therefore, the acute presentation and biopsy results in congruent with the clinical history led us to repeat EUS one month later. This showed a 20 mm by 15 mm irregular mass in the head of the pancreas with upstream pancreatic duct dilation. This time, pathology was sent for flow cytometry and came back positive for lymphoid infiltrate with a preponderance of B-cells surrounded by dense fibrosis and was positive for CD 19, 20, 22 and 10. By this point, malignancy other than adenocarcinoma was suspected and IR guided biopsy of retroperitoneal lymph nodes confirmed a diagnosis of diffuse large B cell lymphoma. Patient started chemotherapy with a 70% chance of being cured. ERCP one month later showed the stricture had resolved and the stent was removed.
Discussion: Keeping a broad differential in mind for pancreatic masses is essential to prevent delayed diagnoses. With that in mind, although rare, pancreatic lymphoma should always be in the differential and physicians should consider sending for flow cytometry to avoid missing this diagnosis. When patients present with recurrent pancreatitis and no risk factors, lymphoma should be kept in the differential.
Disclosures:
Shalini S. Jain, MD1, Faith Abodunrin, MD1, Michael McCabe, MD2. C0062 - Diffuse Large B Cell Lymphoma Presenting as Acute Recurrent Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1CHI Creighton University Medical Center, Omaha, NE; 2Rocky Mountain Gastroenterology Association, Lakewood, CO
Introduction: Extra-nodal Non-Hodgkin’s lymphomas are mostly made of gastrointestinal sites1. Primary pancreatic lymphomas account for < 1% of all extra-nodal lymphomas and are extremely rare. Diagnosis is often missed or delayed due to the prevalence of chronic pancreatitis or pancreatic adenocarcinoma as thought to be the main causes of any pancreatic stricture or mass seen when diagnosing a patient. We present a case of pancreatic lymphoma presenting as acute recurrent pancreatitis.
Case Description/Methods: A 51-year-old male with past medical history of rheumatoid arthritis and nicotine use presented with jaundice, abdominal pain, and fatigue and 30-pound weight loss. MRCP showed intra- and extra-hepatic biliary dilation, showing double duct sign. CT suggested acute pancreatitis. ERCP was done showing a single localized biliary malignant appearing stricture in the lower third of the main bile duct with upstream dilation. EUS showed a 19 mm by 19 mm mass in the head of pancreas and 8 mm dilation of the common bile duct. EUS fine needle biopsy showed chronic pancreatitis with dense fibrosis and benign peri-pancreatic lymph nodes. PET CT showed activity in the pancreas and retroperitoneal lymph nodes. Tumor markers (AFP, CEA, CA 19-9) were within normal limits. Patient had no known risk factors for chronic pancreatitis therefore, the acute presentation and biopsy results in congruent with the clinical history led us to repeat EUS one month later. This showed a 20 mm by 15 mm irregular mass in the head of the pancreas with upstream pancreatic duct dilation. This time, pathology was sent for flow cytometry and came back positive for lymphoid infiltrate with a preponderance of B-cells surrounded by dense fibrosis and was positive for CD 19, 20, 22 and 10. By this point, malignancy other than adenocarcinoma was suspected and IR guided biopsy of retroperitoneal lymph nodes confirmed a diagnosis of diffuse large B cell lymphoma. Patient started chemotherapy with a 70% chance of being cured. ERCP one month later showed the stricture had resolved and the stent was removed.
Discussion: Keeping a broad differential in mind for pancreatic masses is essential to prevent delayed diagnoses. With that in mind, although rare, pancreatic lymphoma should always be in the differential and physicians should consider sending for flow cytometry to avoid missing this diagnosis. When patients present with recurrent pancreatitis and no risk factors, lymphoma should be kept in the differential.
Figure: Figure 1: a) CT showing inflammatory reaction of the pancreas with bile duct dilation; b) Bile duct stricture on ERCP; c) EUS image showing common bile duct stent
Disclosures:
Shalini Jain indicated no relevant financial relationships.
Faith Abodunrin indicated no relevant financial relationships.
Michael McCabe indicated no relevant financial relationships.
Shalini S. Jain, MD1, Faith Abodunrin, MD1, Michael McCabe, MD2. C0062 - Diffuse Large B Cell Lymphoma Presenting as Acute Recurrent Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
